Understanding your child's symptoms
starts here.
When something feels off with your child and you haven’t been able to get clear answers, it’s easy to feel stuck.
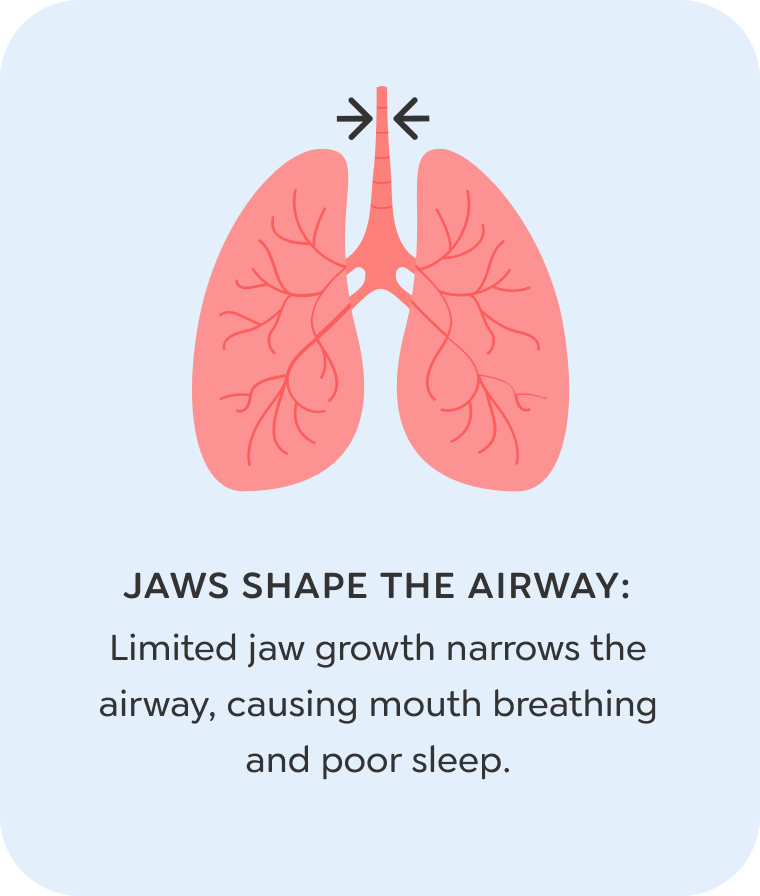
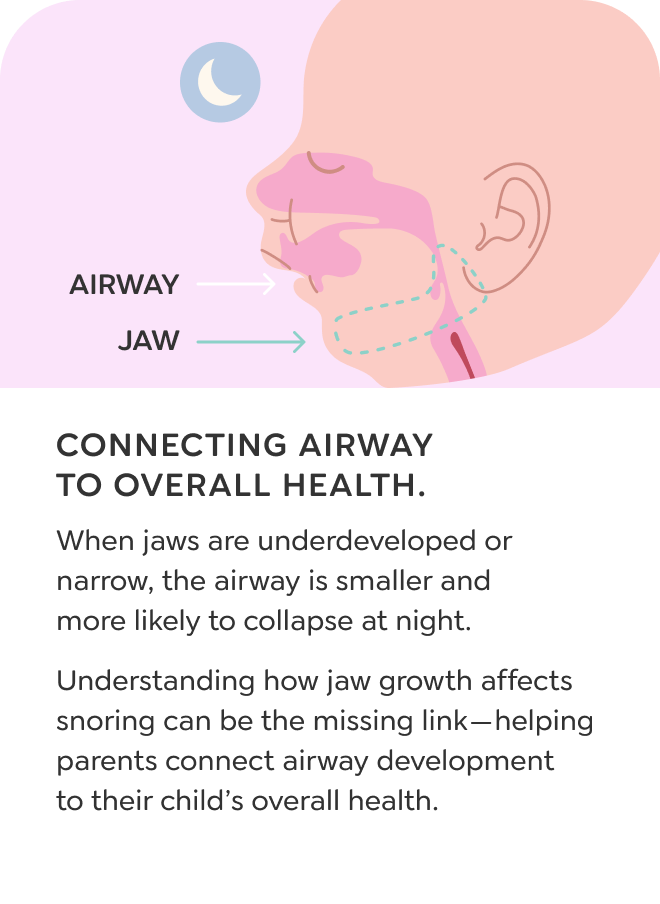
What’s often overlooked is how breathing and jaw development can quietly shape a child’s health, growth, and daily behavior. For many families, it’s the missing piece behind the symptoms no one has been able to explain. Once you see the connection, everything starts to make more sense.
Learn more about the symptoms of airway issues.
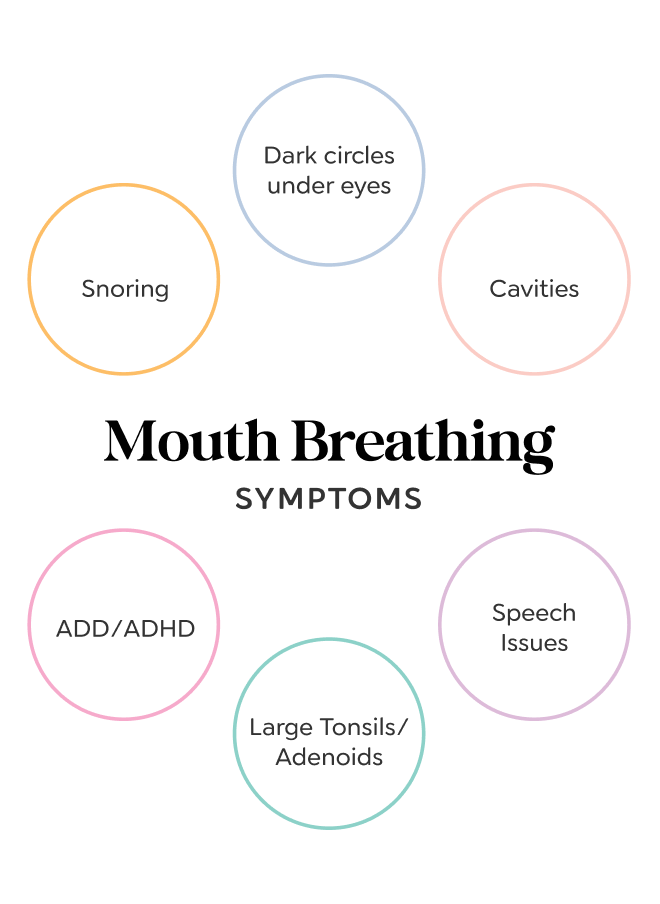
When the airway doesn’t have enough space, the body has to work harder to do simple things—like breathe and sleep. Over time, this can lead to a wide range of symptoms. Some are obvious. Others are harder to connect. But they all matter.
picky eating
My child won't eat anything I give them!
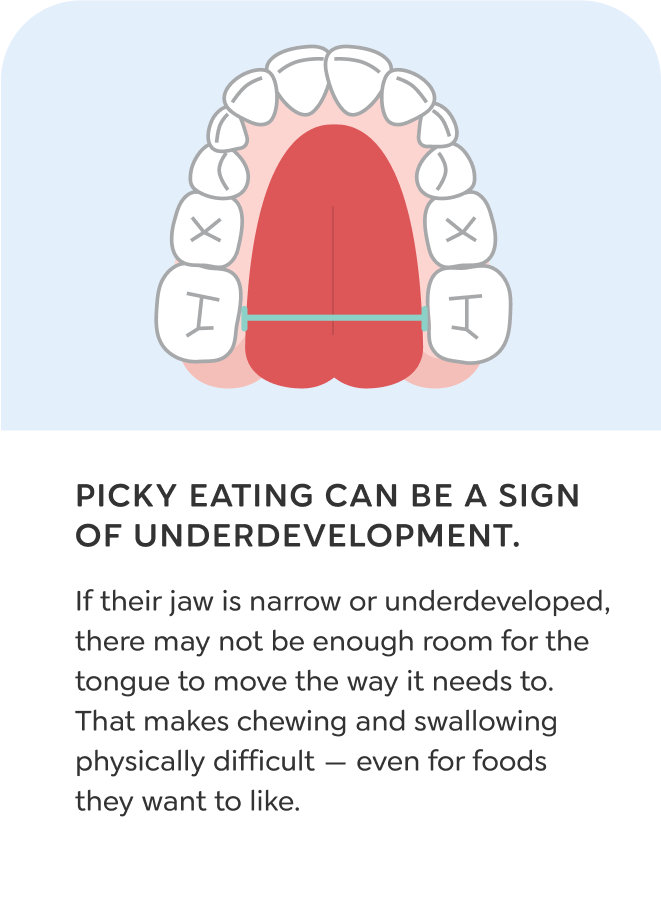
Your child eats fewer than 15 foods, and you’ve tried everything. It’s frustrating — and it’s not your fault. But what if it’s not about behavior? It might be anatomical. And it starts with the mouth and tongue.
Picky Eating
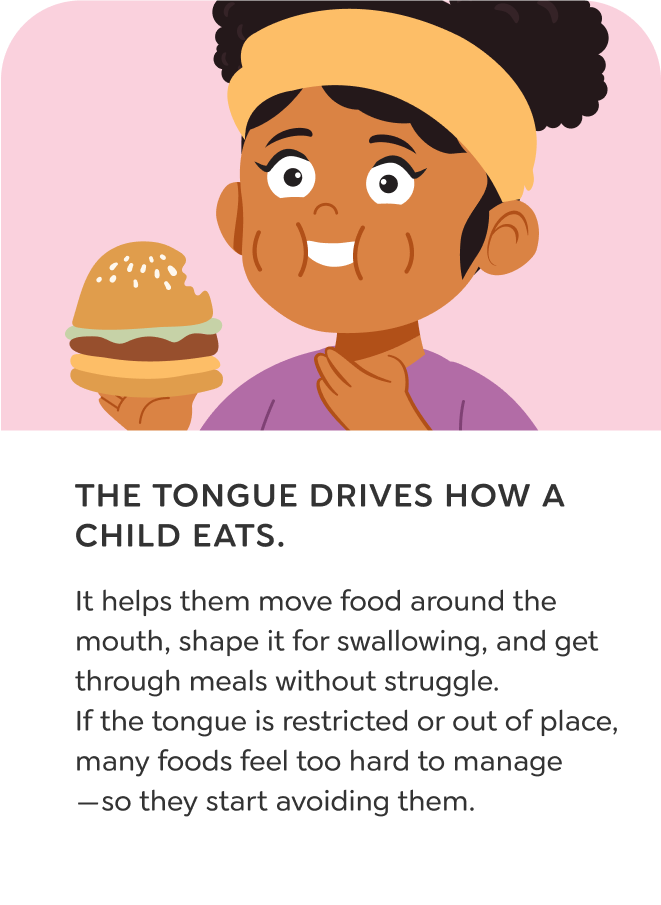
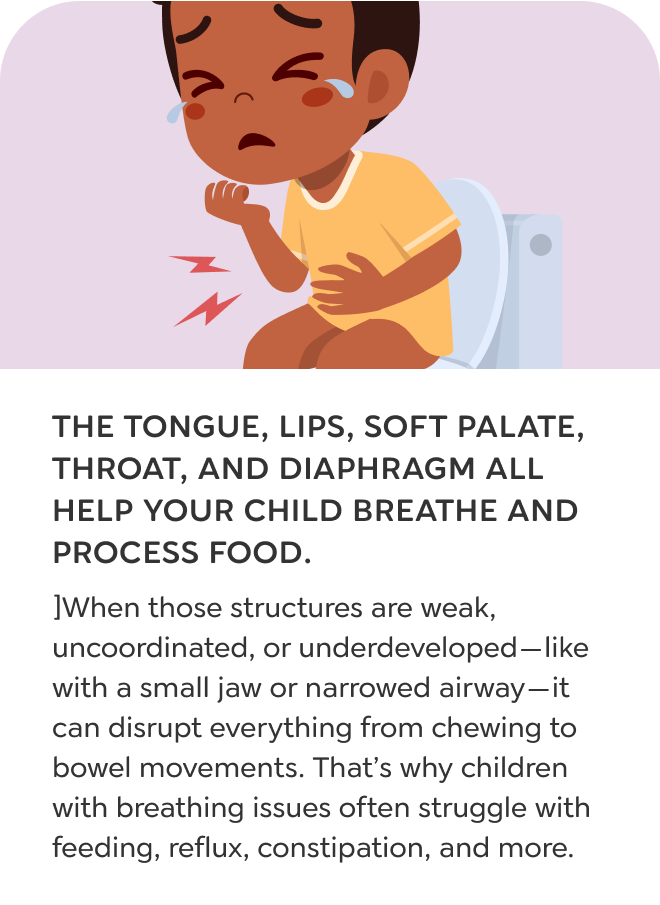
Many children who are labeled as picky eaters aren’t avoiding foods because they’re defiant. They’re avoiding foods that are physically hard to manage. When chewing feels difficult or the tongue doesn’t function well, a child will naturally prefer soft, bland options that require less effort. What seems like preference is often the result of oral muscles that didn’t develop the strength or coordination needed for harder textures.
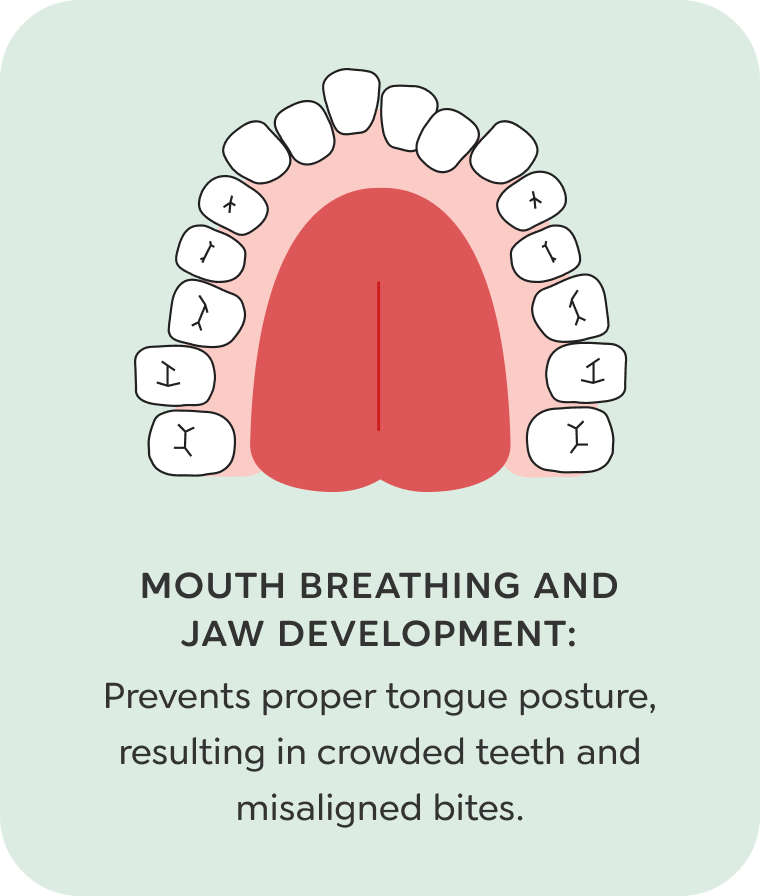
This usually starts in infancy. If a child spends a long time eating purees or soft foods, the tongue muscles don’t get the training they need. Without proper strength or movement, the tongue tends to sit low in the mouth and can’t guide or clear food effectively. Jaw development may also be limited, especially in children who breathe through the mouth instead of the nose.
As the mouth struggles to manage more challenging textures, the range of accepted foods narrows. Picky eating is often one of the earliest signs that the muscles and structures used for eating didn’t develop the way they should.
Speech Issues
My child struggles to speak clearly!
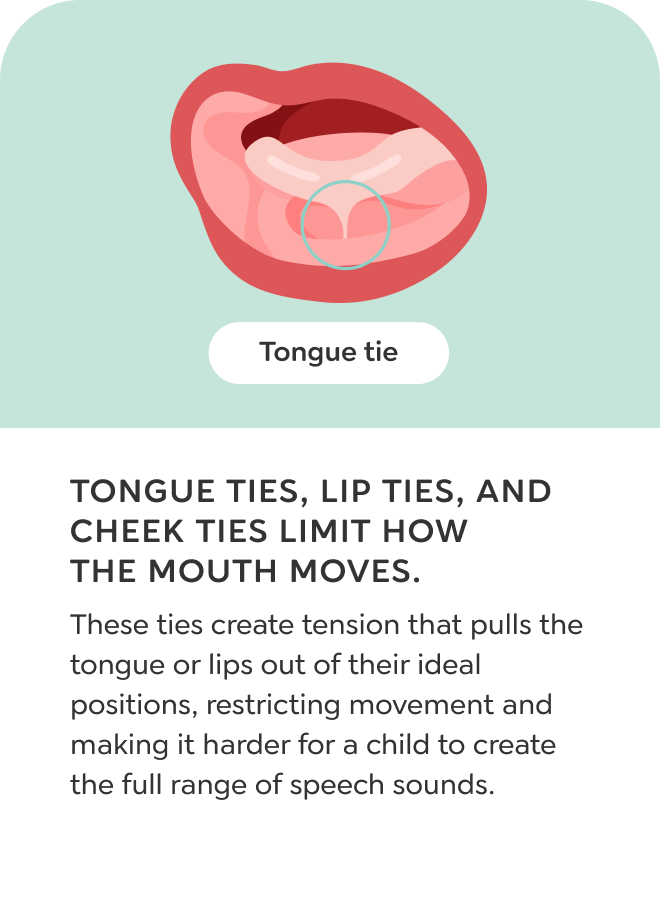
Your child mixes up sounds or avoids certain words, and speech therapy isn’t fully helping. A crowded mouth or small jaw might be limiting tongue movement. That can make speech less clear even when the brain knows what to say.
Speech Issues
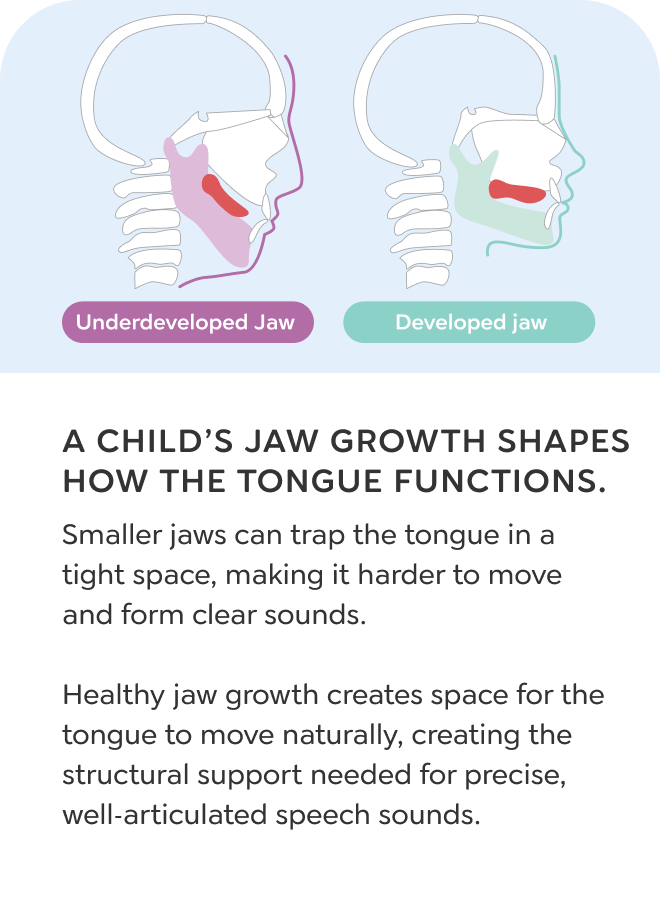
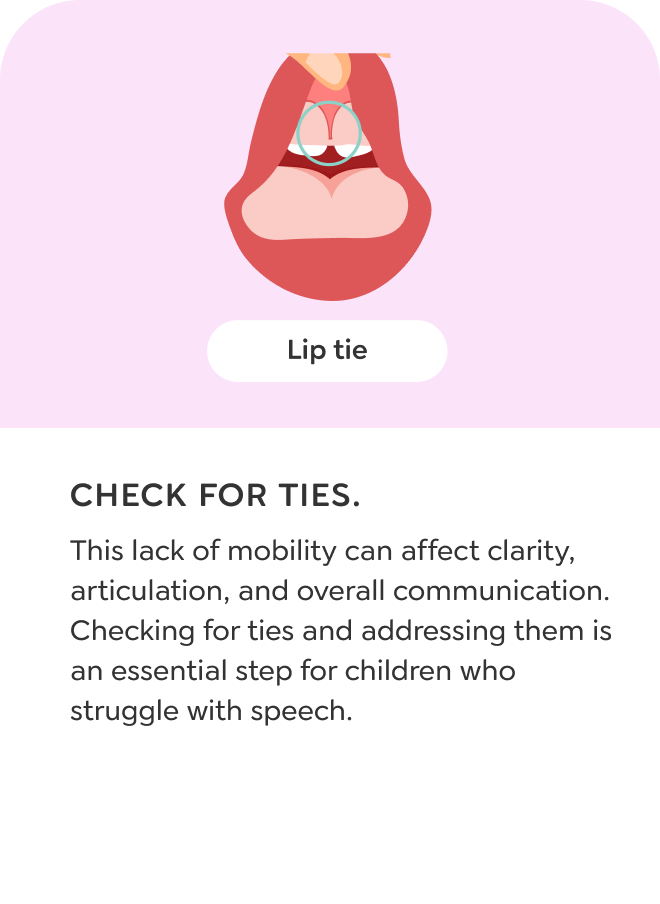
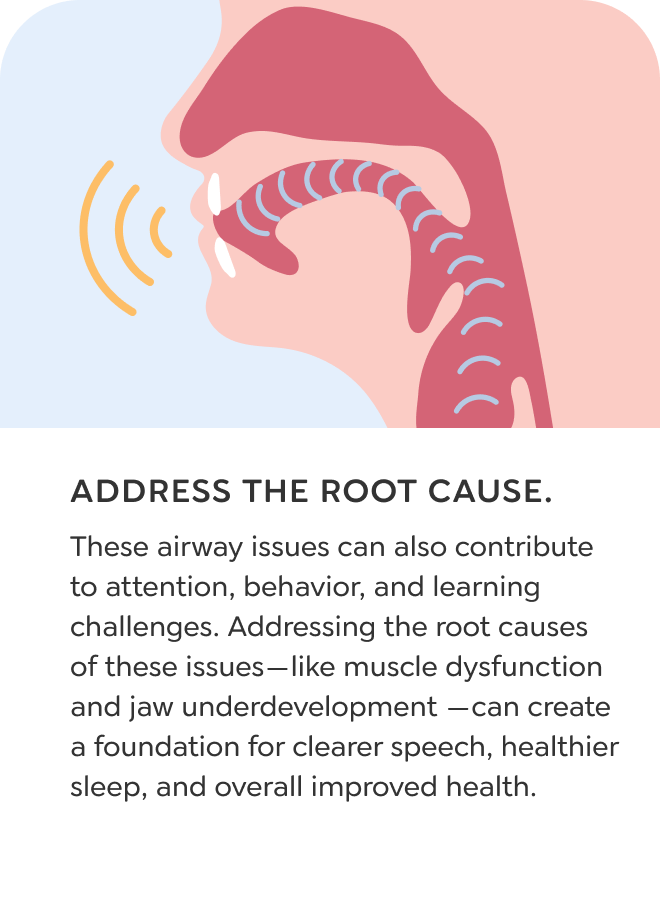
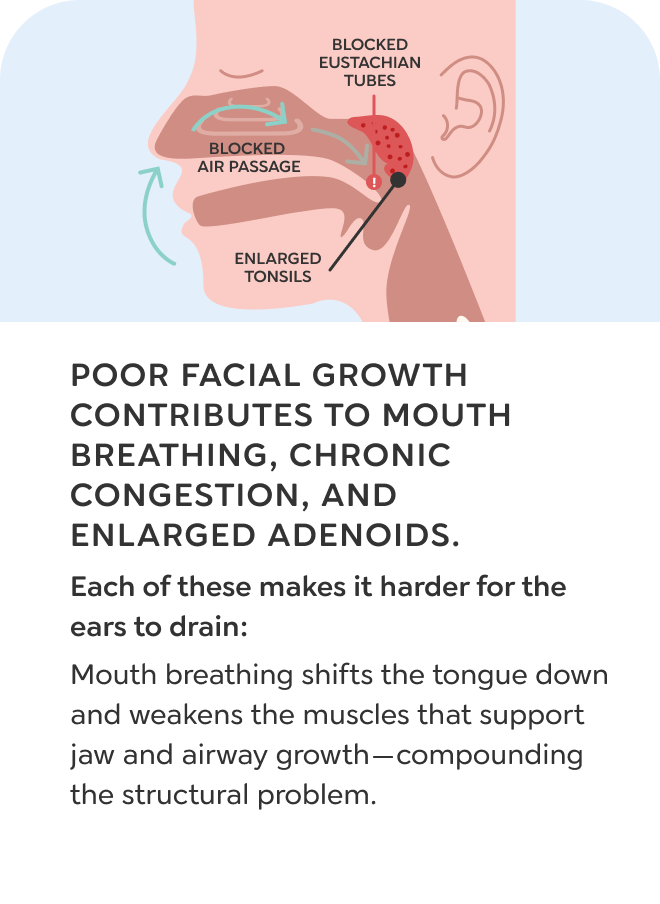
Some children struggle to speak clearly because their mouth doesn’t give the tongue enough space to move. When the jaws are small or underdeveloped, the oral cavity becomes too crowded. A normal-sized tongue working in a smaller space has trouble reaching the right positions for clear sounds. This can make it harder to pronounce letters like L, R, S, SH, or TH. Underdeveloped jaws can also affect the angle of the Eustachian tubes, making it harder for fluid to drain properly. When drainage is poor, hearing can be reduced—and hearing loss during early development often delays speech. Chronic nasal congestion and narrow airways can also change how a child sounds, especially if the voice is nasal or muffled. Ties in the tongue, lips, or cheeks can further limit the precise movements needed for clear articulation.
These physical limitations affect both how children produce sounds and how they hear them. While speech therapy can help, long-term progress often depends on whether the mouth, tongue, and airway are functioning the way they should.
SNORING
My child snores, even when they’re not sick!
Your child breathes loudly at night, and it keeps happening even when they’re healthy. It’s not just noise. Snoring tells us the airway is tight. The tongue, jaws, or tonsils may be making it harder to breathe during sleep.
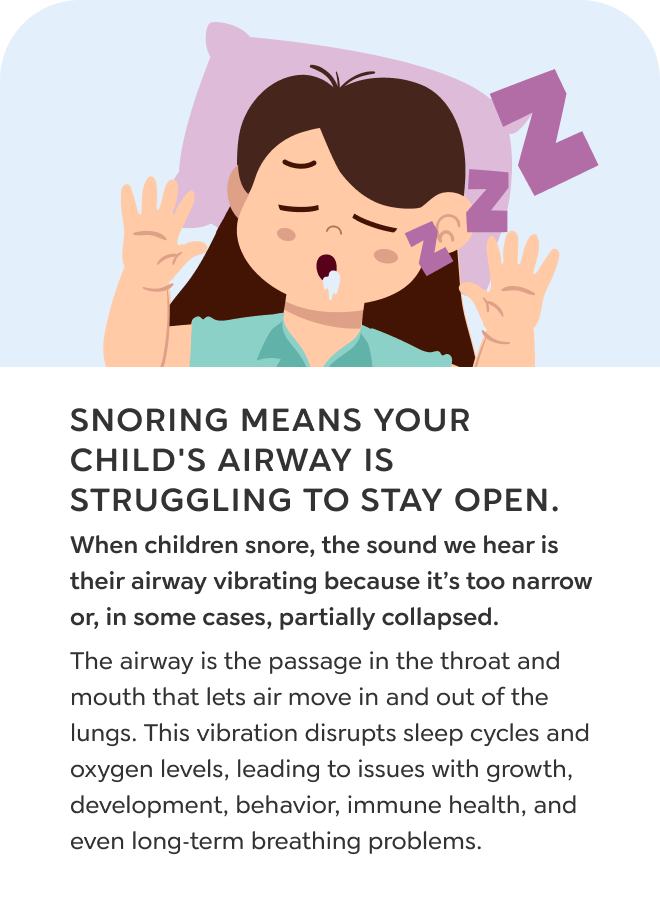
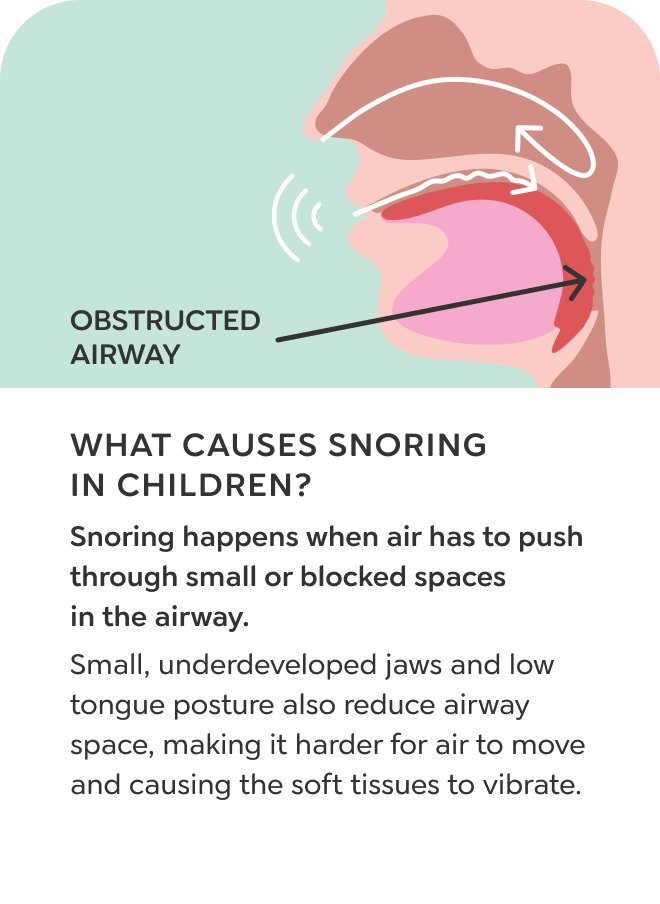
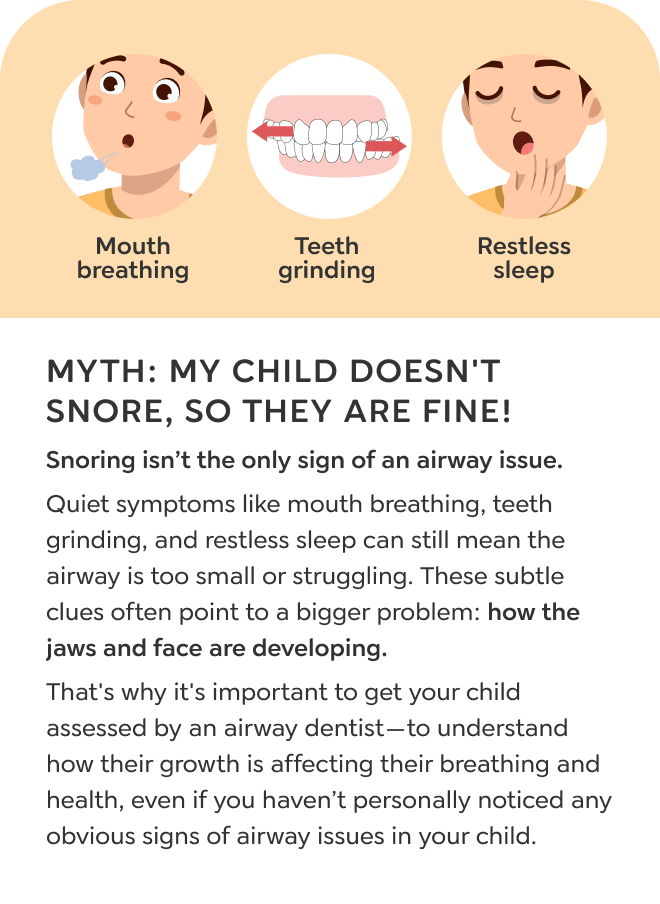
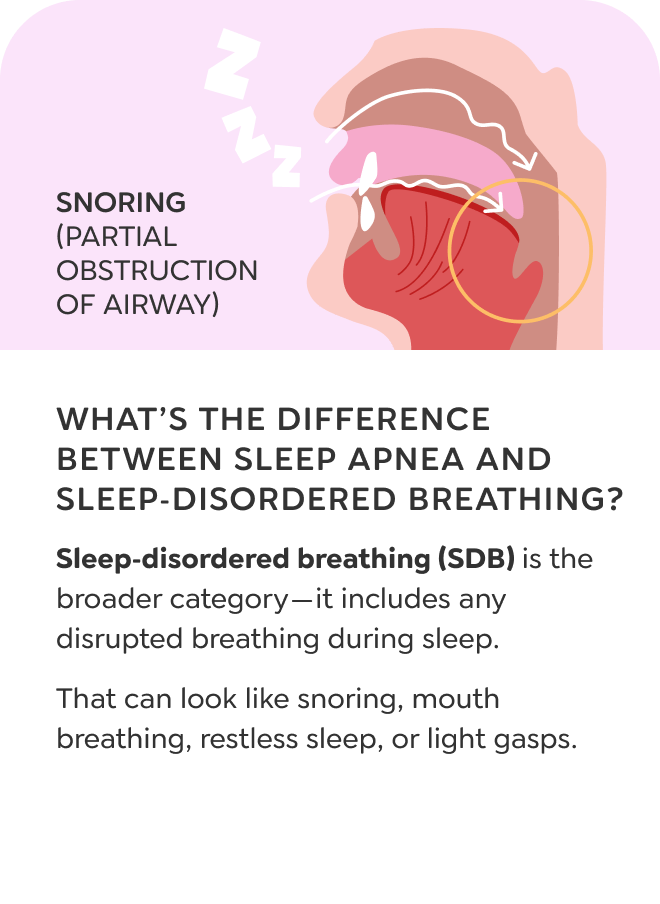
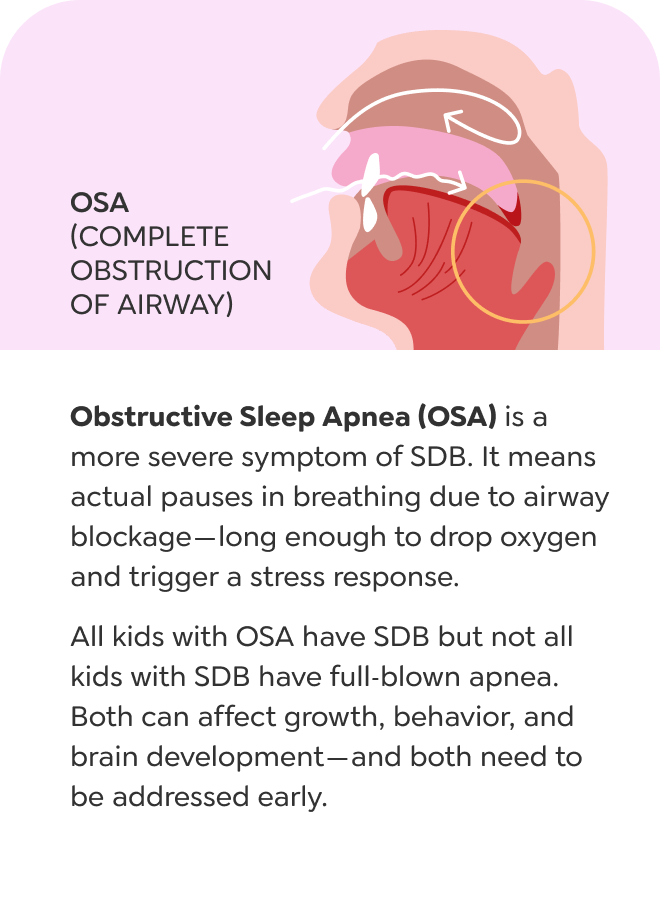
Snoring
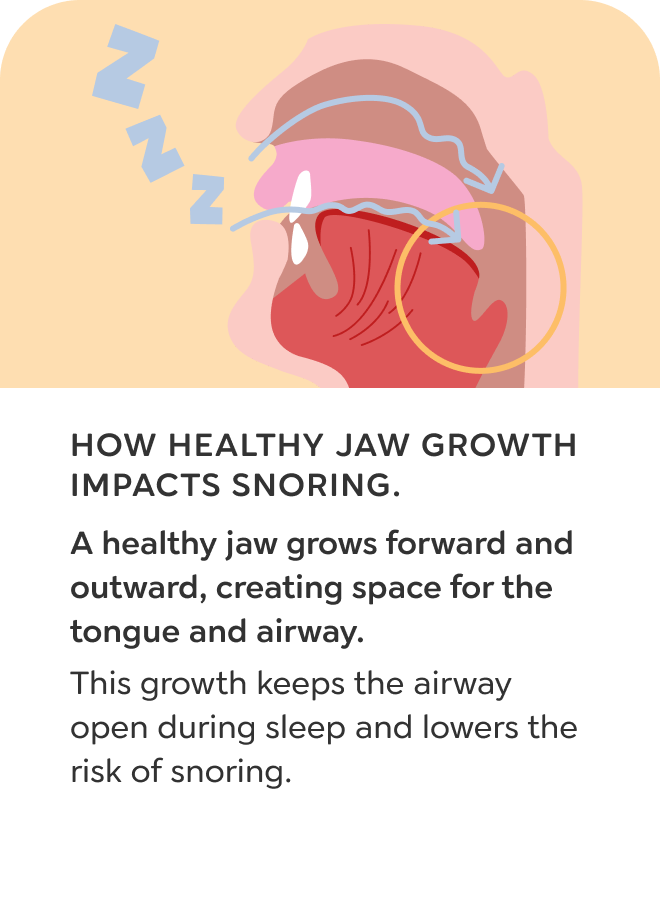
Snoring in children is a sign that the airway is physically too narrow for healthy breathing. As air moves through a restricted space during sleep, it causes soft tissue in the throat to vibrate. That vibration means airflow is being forced through a small space, increasing resistance and putting strain on the body’s ability to breathe.
Snoring often reflects a structural issue. When the upper and lower jaws don’t grow forward enough, there isn’t enough space for the tongue or the airway. If the tongue falls back during sleep or the tonsils are enlarged, the airway becomes even smaller and more prone to collapse.
Snoring is one form of sleep-disordered breathing. Every episode of snoring causes a drop in airflow, triggering the brain to interrupt sleep and restore breathing. These disruptions prevent the body from reaching the most restorative stages of sleep and can impact growth, hormone production, behavior, attention, and immune function—even if your child appears to sleep through the night.
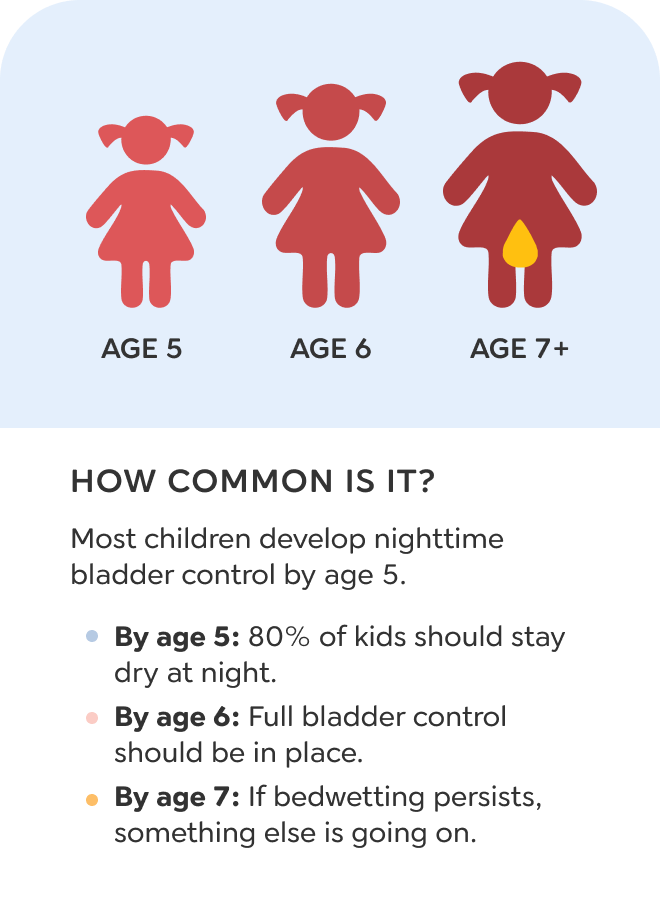
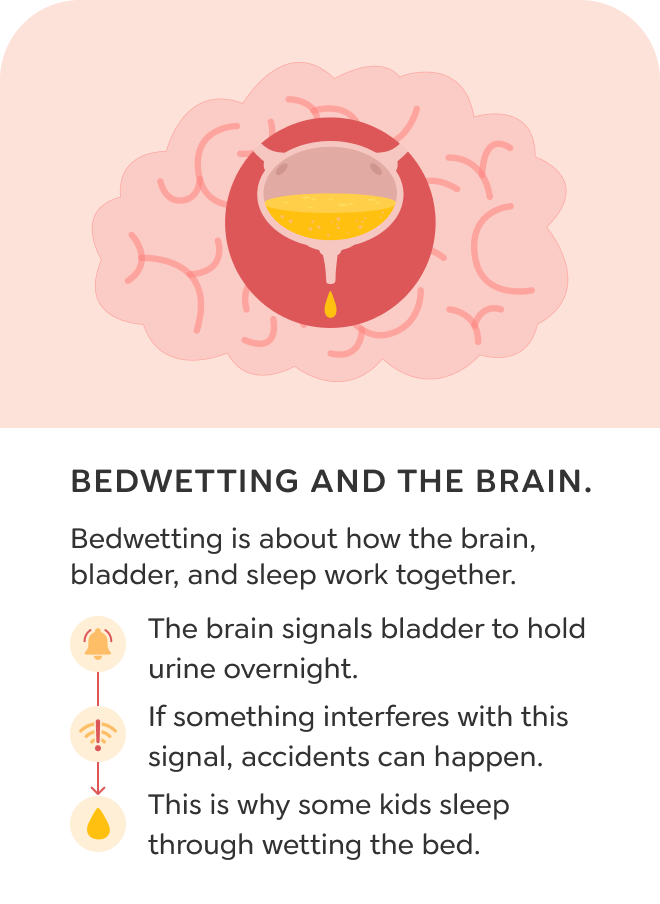
BEDWETTING
My child still wets the bed almost every night!
Your child seems old enough to stay dry, and accidents no longer make sense. It’s not always about maturity. If breathing is strained at night, the nervous system can struggle to regulate bladder control during sleep.
Bedwetting
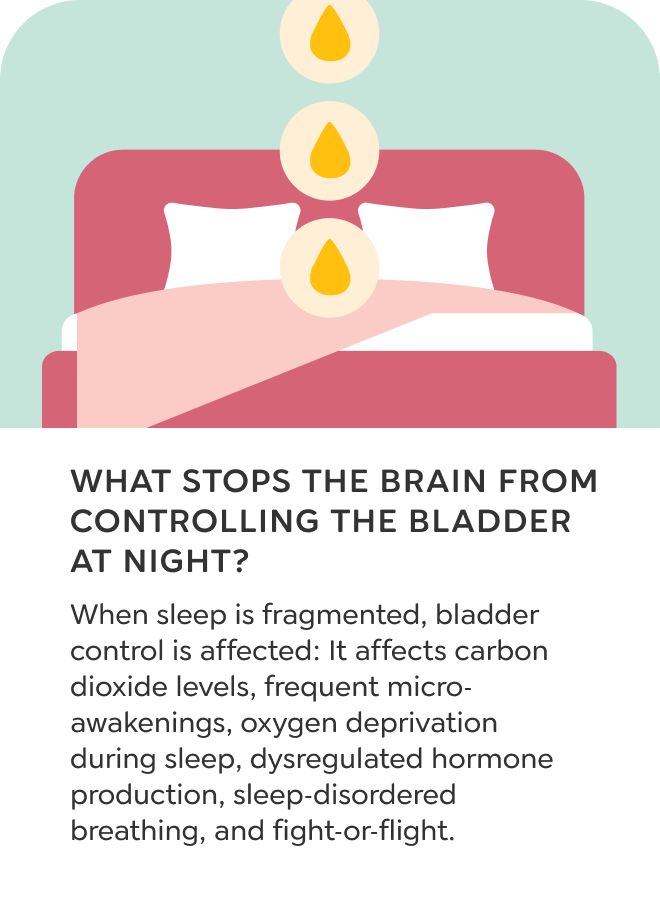
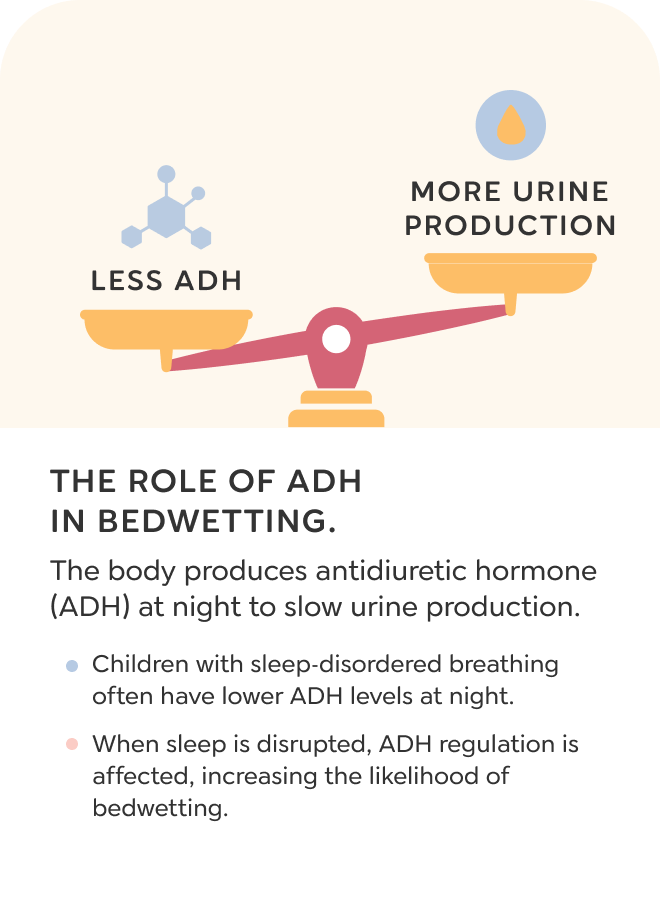
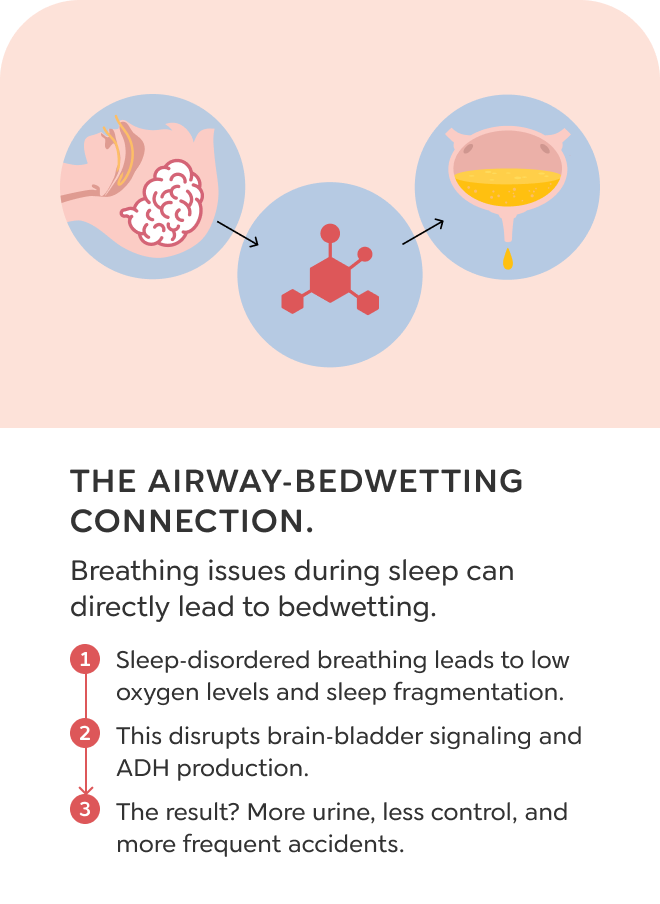
Chronic bedwetting is often labeled a behavioral or developmental issue, but many children experience it because of disrupted sleep and poor breathing. When a child struggles to breathe well at night, the brain shifts into a stress state. This fight-or-flight response deprioritizes the urinary system, making it harder for the body to regulate bladder control during sleep.
Mouth breathing, snoring, or airway obstruction can also raise heart rate and blood pressure. That increased circulation requires more filtering, which leads to more urine production overnight. At the same time, the child may not be in a deep enough sleep cycle to fully wake and use the bathroom. Instead, the body releases urine as a protective response.
A third pathway involves body temperature. Children with poor nighttime breathing often move constantly in their sleep. That activity raises internal temperature, and one of the body’s natural cooling methods is urination. Bedwetting is not always about maturity. It is often a sign that sleep quality is compromised and the nervous system is working around poor airway function.
ADD / ADHD
My child can’t focus or sit still!
Your child bounces between tasks, acts impulsively, or seems constantly restless. Poor sleep can overstimulate the nervous system. What looks like attention issues may start with breathing problems at night.
ADD / ADHD
Children diagnosed with ADD or ADHD often show behaviors that overlap with chronic sleep deprivation. Difficulty focusing, impulsivity, hyperactivity, and poor emotional regulation are all common signs when the brain isn’t getting the deep sleep it needs. These symptoms are not always the result of a neurological condition. In many cases, they begin with disrupted breathing during sleep.
When the jaws are underdeveloped, there may not be enough room for the tongue or airway. This can lead to fragmented sleep as the brain works to keep the airway open throughout the night. Even if the child appears to sleep through, they may never reach the deepest stages of rest. That constant disruption affects how the brain functions during the day.
Behavior challenges that seem rooted in attention may actually reflect a structural issue that starts with the airway. Without deep, consistent sleep, the nervous system cannot regulate properly. What looks like ADHD may be the outward sign of a child whose body is struggling to rest and recover.
CROOKED TEETH
My child’s teeth are coming in all over the place!
Your child’s baby teeth look tight, or the adult ones came in crooked. This isn’t just genetic. A narrow dental arch means less space for teeth. It often means less space for the tongue and airway too.
Crooked Teeth
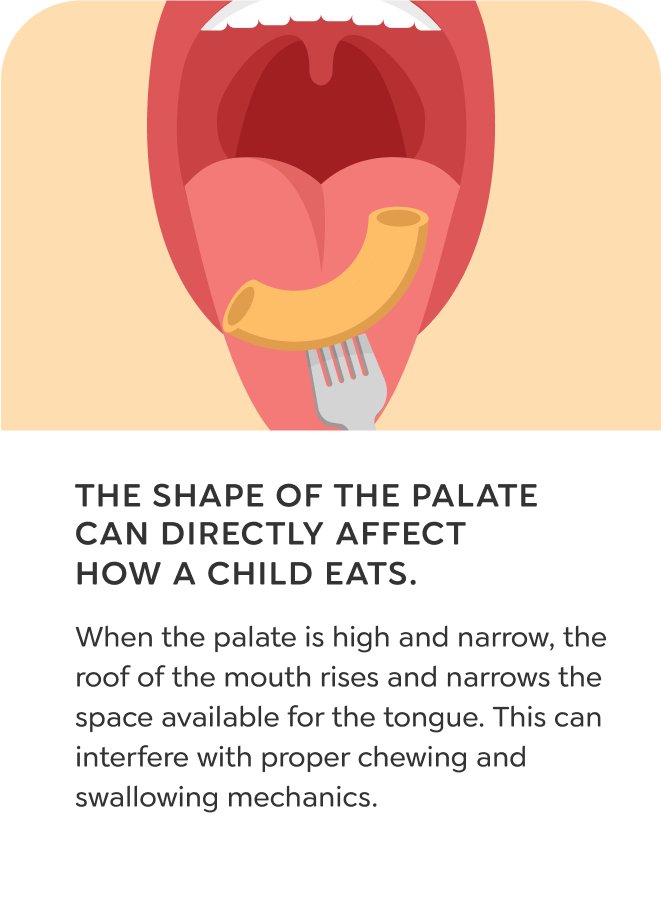
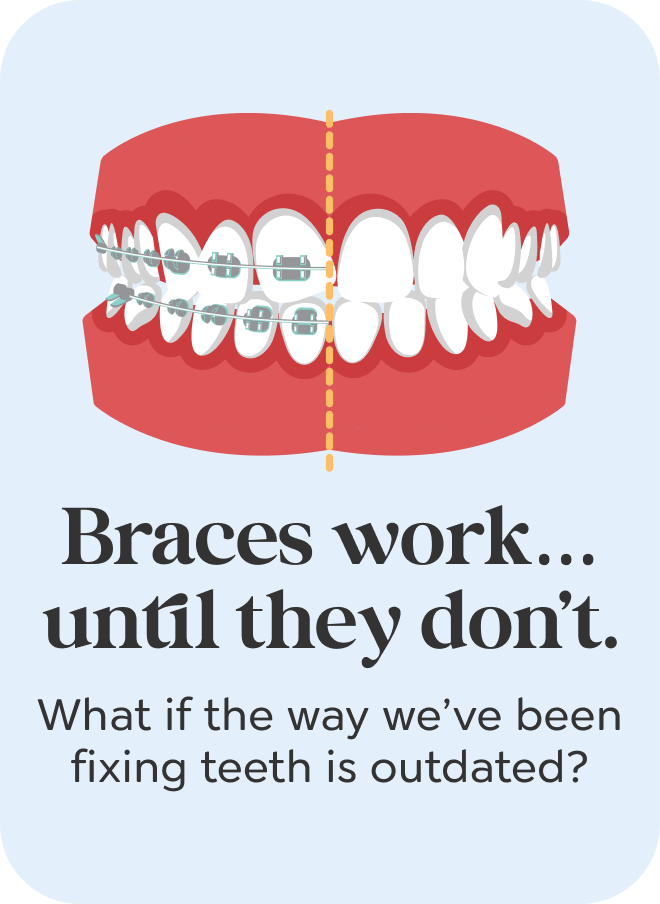
Teeth become crowded when the jaws are too small to fit them. This isn’t caused by the teeth themselves—it starts with how the face and jaws are developing in early childhood. One of the first signs is tight baby teeth with little or no space between them. Without enough room, the larger permanent teeth erupt crooked, overlapped, or rotated.
The upper jaw, or palate, is shaped by the tongue pressing against it during rest. If the tongue sits low in the mouth or the child breathes through the mouth instead of the nose, the palate stays narrow and the dental arch doesn’t widen the way it should. When forward growth is also restricted, the jaws become too small for both the teeth and the airway.
Crooked teeth are often the earliest visible sign of underdeveloped jaws. They tell us that growth has not kept up with the body’s needs. Small jaws also leave less space for the tongue and airway, increasing the risk of mouth breathing, poor sleep, and long-term health effects.
NIGHT TERRORS
My child screams in their sleep and won’t wake up
Your child cries or panics at night but doesn’t remember it by morning. Instead of cycling through sleep normally, they may be stuck in shallow stages. This often happens when breathing gets disrupted during deeper sleep.
Night Terrors
Night terrors are episodes where a child may cry out, sit up, or appear terrified during sleep, often without waking or remembering the event. These episodes tend to occur in the first half of the night, during transitions between sleep stages. While they are often labeled as neurological, many are triggered by sleep fragmentation caused by poor breathing.
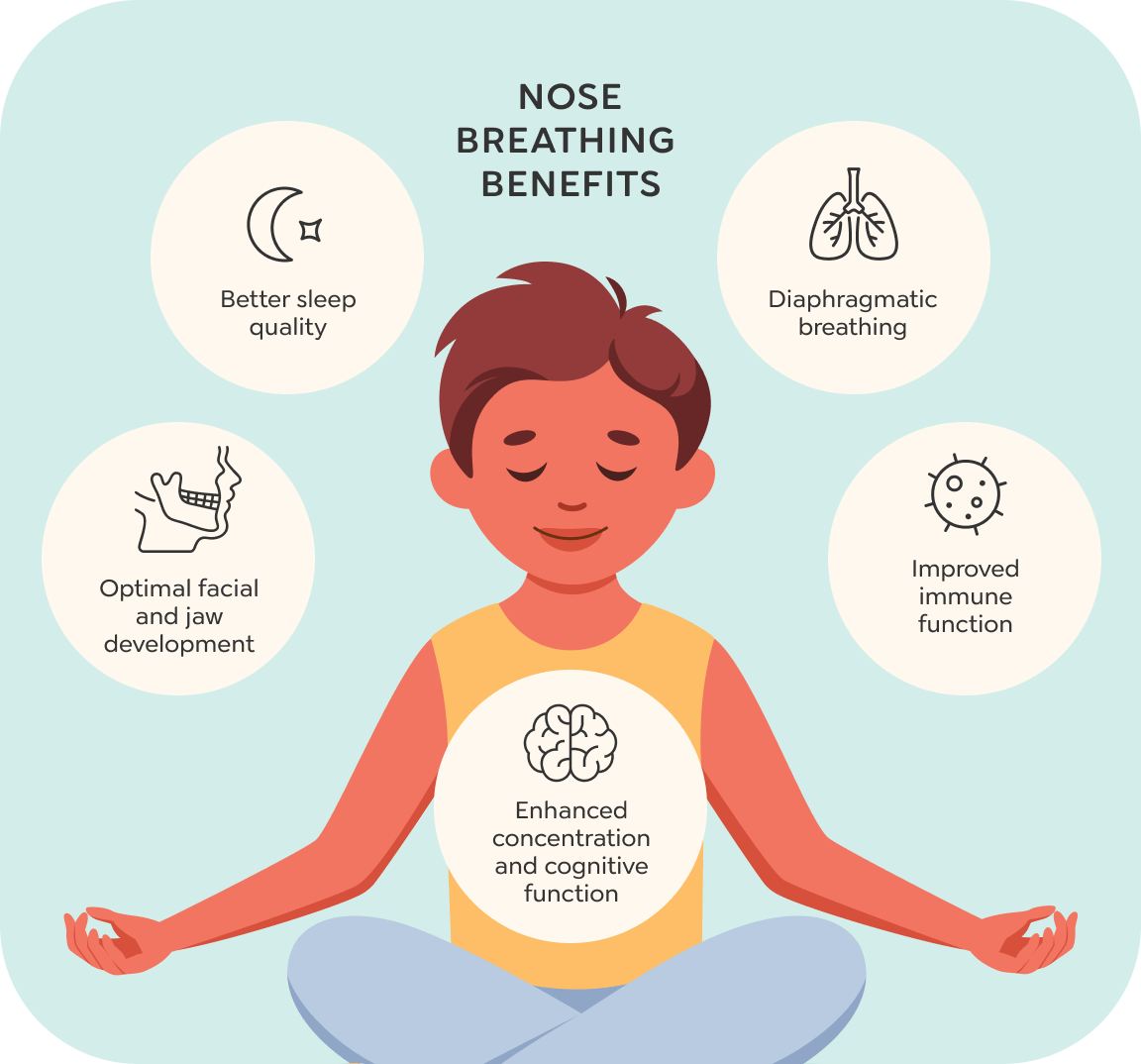
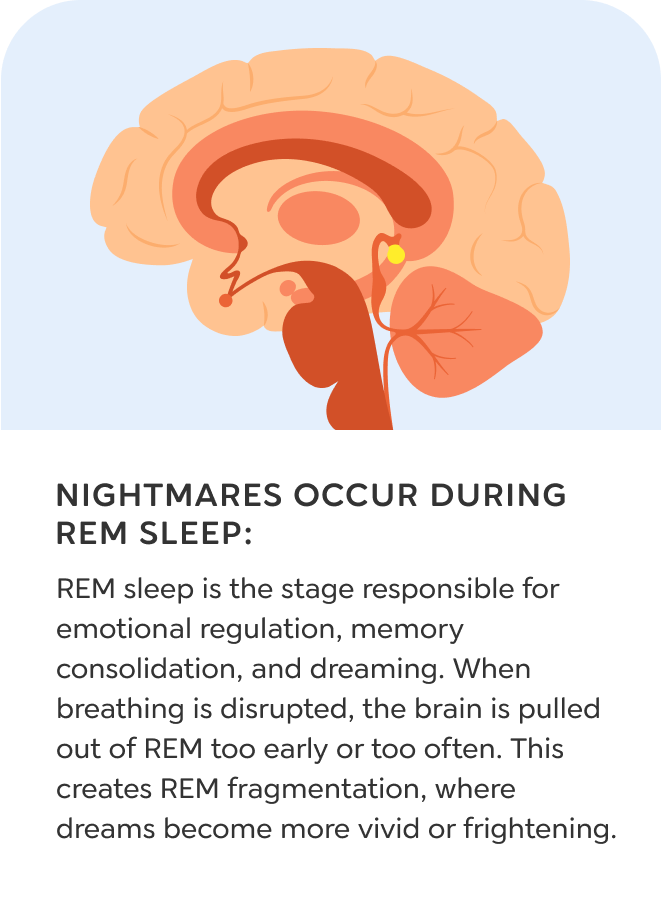
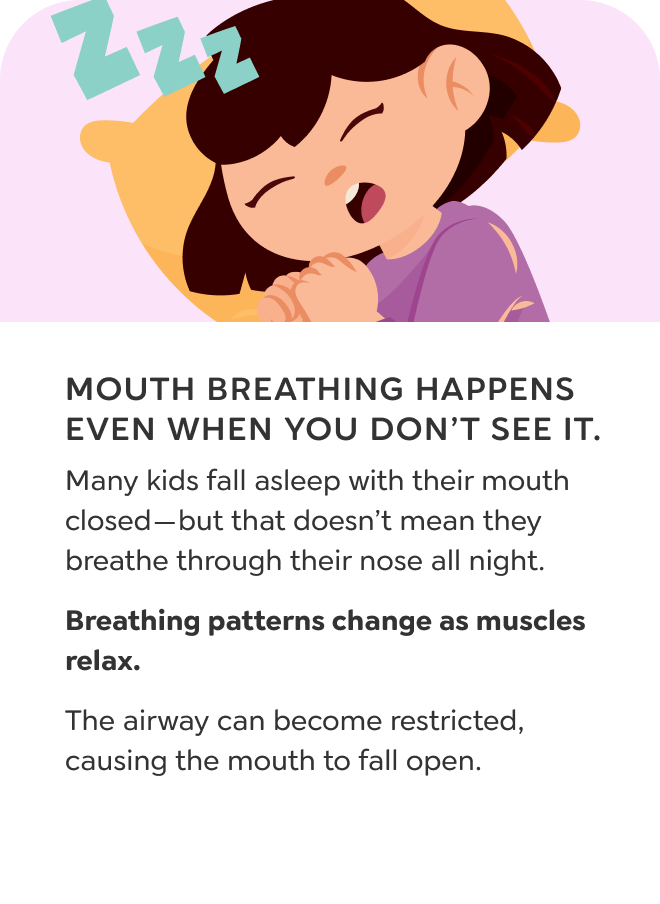
Children who breathe through their nose at night are more likely to move smoothly through each sleep stage, including deep sleep and REM, where dreaming occurs. But children who mouth breathe often struggle to maintain stable sleep cycles. As airflow becomes disrupted, the brain stays partially alert to keep breathing steady. That instability fragments the sleep cycle and interferes with dreaming.
Instead of entering REM sleep, the child may partially awaken in a disoriented state, resulting in a night terror. This is not a behavioral issue—it is often a physiological response to broken sleep. Addressing the root cause of mouth breathing can help restore more stable sleep and reduce the frequency of night terrors.
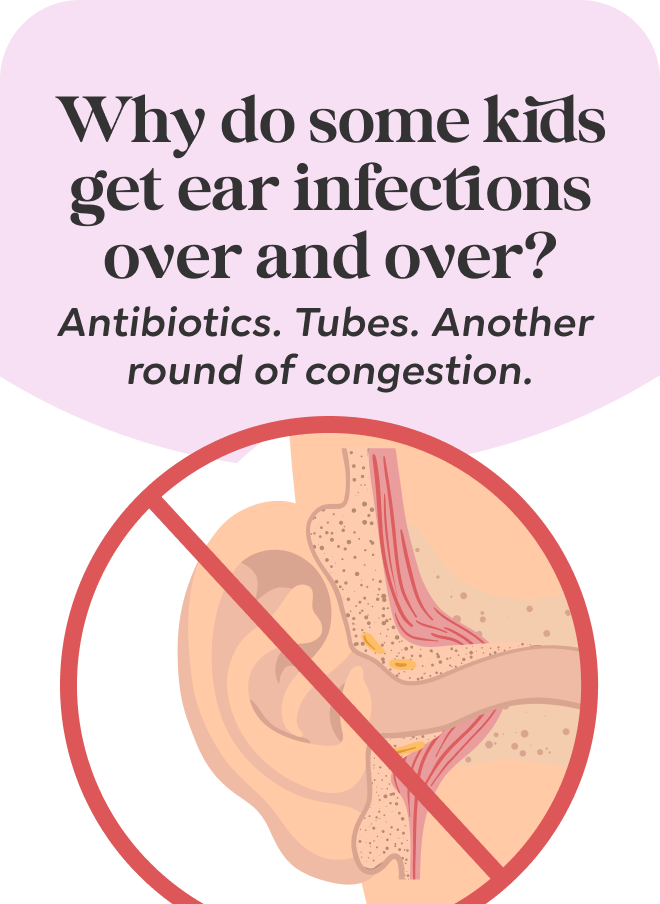
EAR INFECTIONS
My child keeps getting ear infections, even after tubes!
Your child has had round after round of ear issues, and nothing seems to stick. If the tongue rests low or swallowing isn’t strong, fluid can build in the ears. That fluid sets the stage for chronic infection
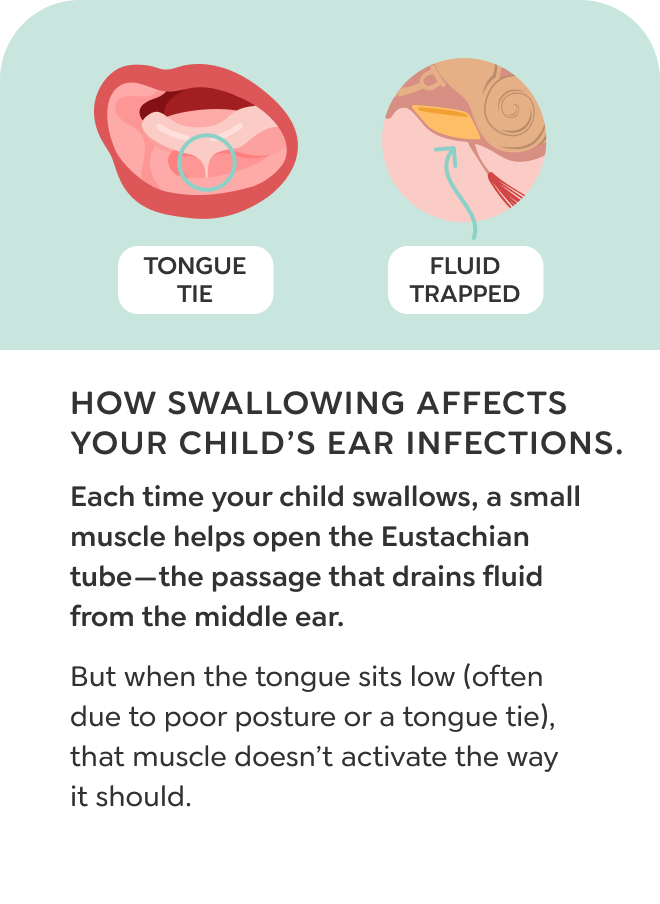
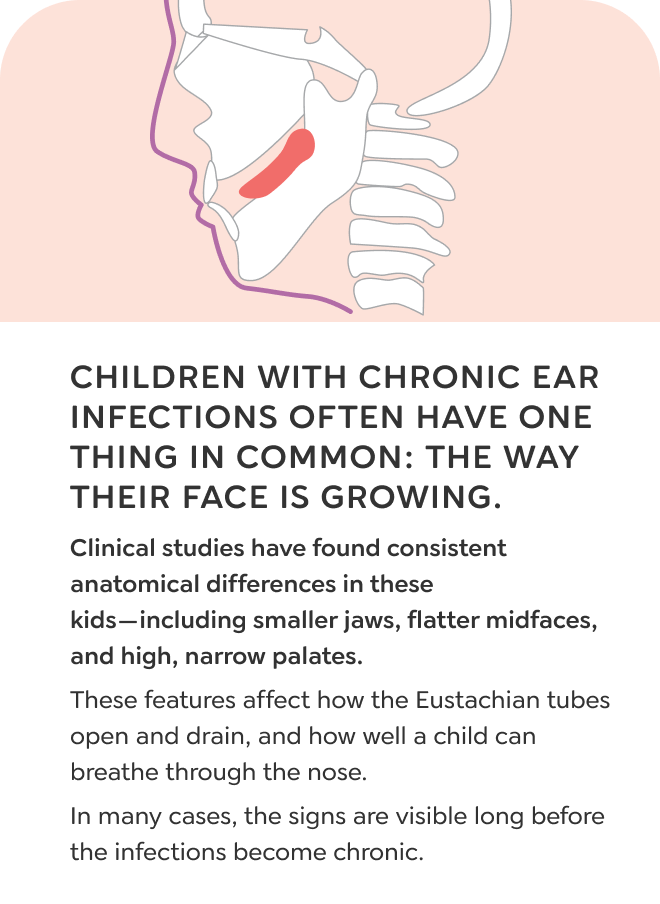
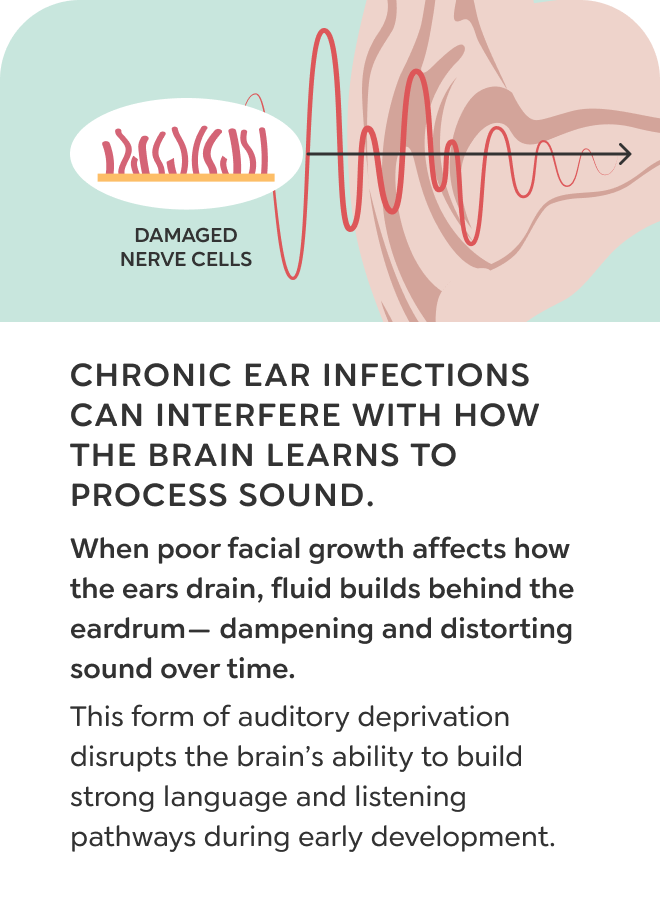
Ear Infections
Recurring ear infections are rarely just an issue with the ears. They often begin when fluid collects in the middle ear and doesn’t drain properly. That stagnant fluid becomes a breeding ground for bacteria, which leads to infection. The real question is not why the ear becomes infected, but why the fluid is stuck in the first place.
Fluid from the middle ear drains through the Eustachian tube, which opens during a proper swallow. This process relies on the tongue rising to the roof of the mouth to activate the surrounding muscles. Children who breathe through their mouth or have low tongue posture often develop dysfunctional swallowing patterns. Instead of pressing upward, the tongue moves side to side or falls back. As a result, the muscles that open the Eustachian tube are never engaged, and fluid stays trapped.
Antibiotics and ear tubes may relieve symptoms temporarily, but they don’t address the cause. When swallowing and tongue posture are not corrected, fluid continues to build. That’s why the infections often return.
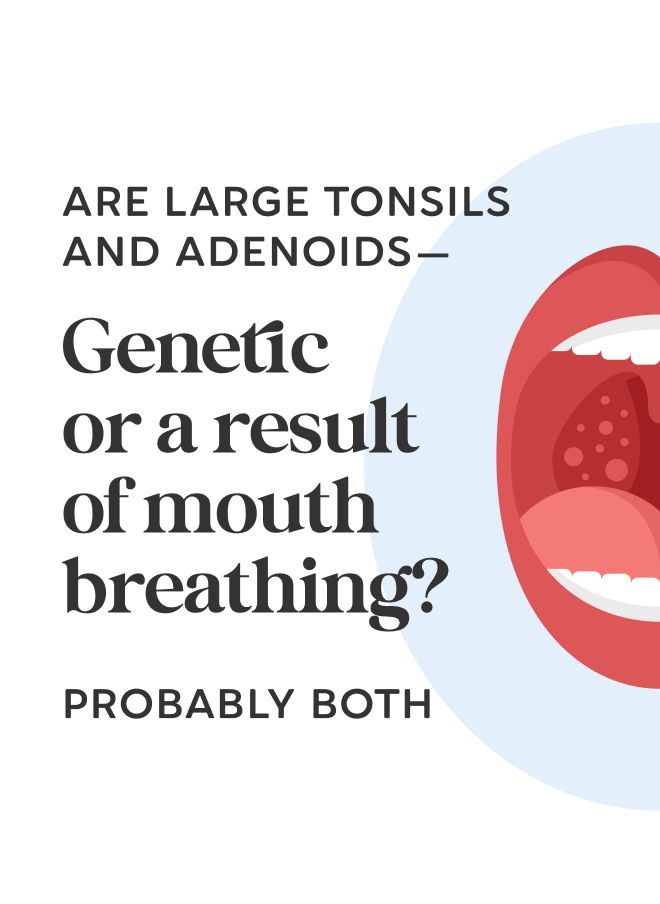
LARGE TONSILS & ADENOIDS
My child’s tonsils are always swollen!
Your child has puffy tonsils or adenoids that just won’t calm down. But what if they’re not the cause? Swelling may be the result of mouth breathing or poor drainage. The airway might already be under strain.
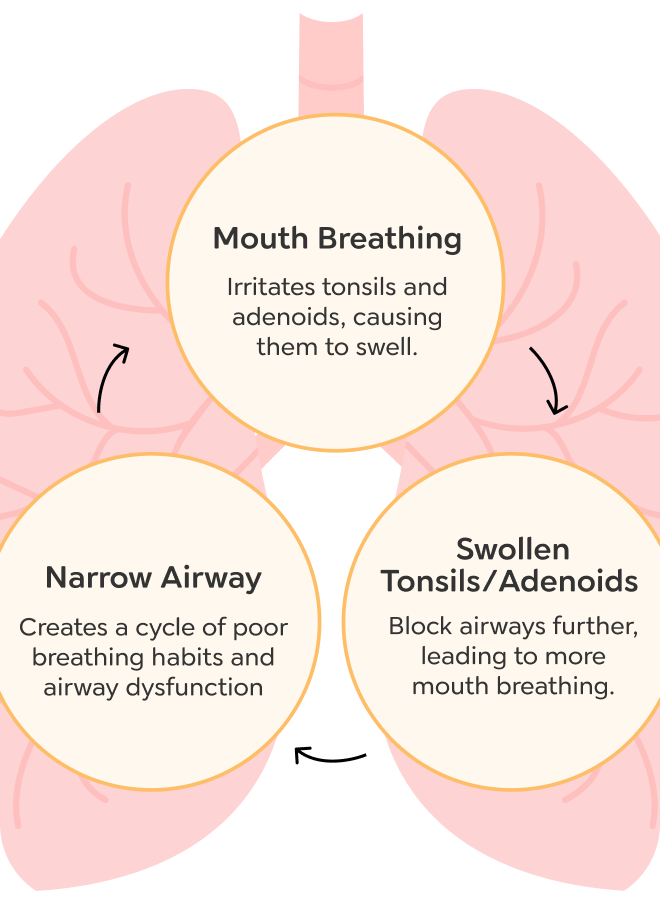
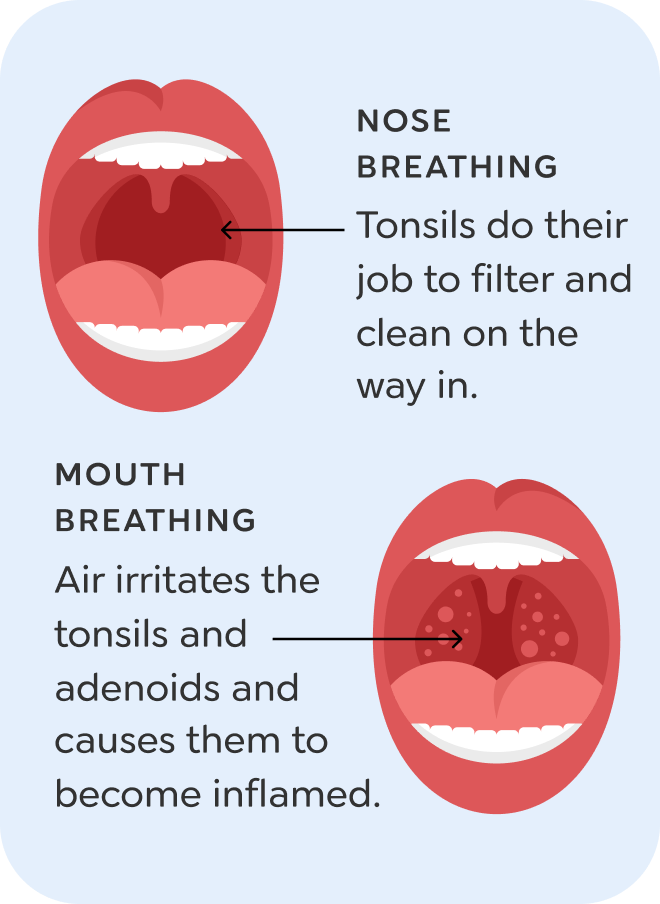
Large Tonsils & Adenoids
Large tonsils and adenoids are often blamed for airway problems, but in many cases, they are a result of poor breathing, not the cause. These tissues tend to enlarge when a child starts breathing through the mouth. Mouth breathing brings dry, unfiltered air into the throat, which irritates the tonsils and adenoids and causes them to swell.
This often begins with underdeveloped jaws that limit space for the tongue and make nasal breathing more difficult. As the child shifts to mouth breathing, the body uses the chest muscles instead of the diaphragm to breathe. Without the normal movement of the diaphragm, the lymphatic system slows down. This prevents the tonsils and adenoids from draining properly, which adds to the swelling.
Tonsil and adenoid removal may relieve the blockage, but it does not address the cause of the problem. If jaw growth, tongue posture, and nasal breathing are not corrected, the airway remains compromised. That can lead to ongoing issues with sleep, speech, and overall health.
CAVITIES
My child keeps getting cavities, even with great hygiene!
Your child brushes well, eats healthy, and still gets decay. The issue might be dry mouth. If they breathe through the mouth, saliva dries up. That leaves teeth exposed to acid and bacteria with no protection.
Persistent Cavities
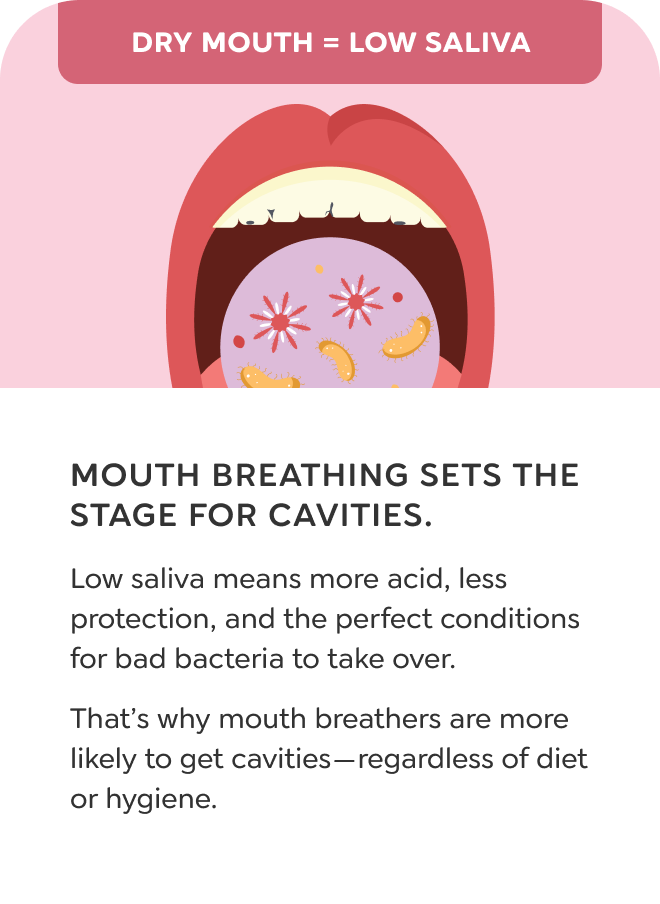
Persistent cavities are often linked to mouth breathing, not just brushing or diet. Even with consistent hygiene and low sugar intake, children who breathe through their mouth are more likely to develop decay because of how it disrupts the oral environment.
Mouth breathing dries out the teeth and reduces saliva. Saliva is essential for protecting enamel, neutralizing acid, and washing away food particles. When the mouth stays open during the day or night, that saliva barrier is lost. Without it, bacteria and acid have direct contact with the teeth for longer periods.
Airflow through the mouth also changes the balance of oral bacteria. Harmful bacteria thrive in dry, oxygen-exposed environments. As the protective system breaks down, cavities become more common and harder to prevent.
>When a child has frequent cavities despite good brushing and a healthy diet, the problem may not be dental hygiene. It is often a sign that the child is breathing through the mouth, especially during sleep, and that the structures supporting nasal breathing need to be evaluated.
HEADACHES
My child keeps waking up with headaches!
Your child starts the day with pressure or pain behind the eyes. Poor sleep and low oxygen can strain the brain. If breathing is off at night, the nervous system stays tense. That tension can lead to morning headaches.
Headaches
Headaches in children can have many causes, but when they appear alongside poor sleep, mouth breathing, or fatigue, it may point to airway dysfunction. A child with underdeveloped jaws often struggles to breathe well at night, which disrupts their sleep and reduces oxygen flow to the brain. That disruption affects how the brain regulates pain and recovers overnight.
Instead of reaching deep, restorative sleep, the nervous system stays activated, the brain remains unrested, and inflammation builds. This can result in morning headaches, dull pressure behind the eyes, or discomfort that comes and goes throughout the day. The child may not always describe it as a headache. They may say they feel tired, irritable, or want to avoid light and sound.
If a child has headaches alongside signs like snoring, grinding, or mouth breathing during sleep, it may be a sign that their airway is not supporting healthy breathing. Addressing the root cause can improve oxygen levels, sleep quality, and pain sensitivity throughout the day.
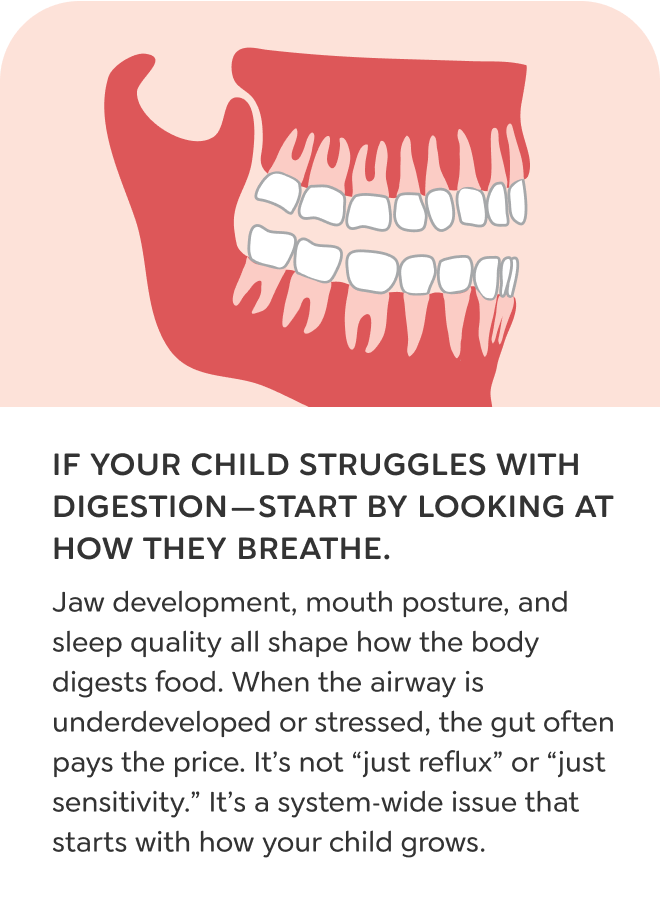
DIGESTION
My child always complains of a stomachache!
Your child wakes up queasy, gets gassy after meals, or avoids food. Swallowing extra air and missing out on restful sleep can throw digestion off balance. Poor airway function might be interfering with how the gut processes and recovers.
Digestive Issues
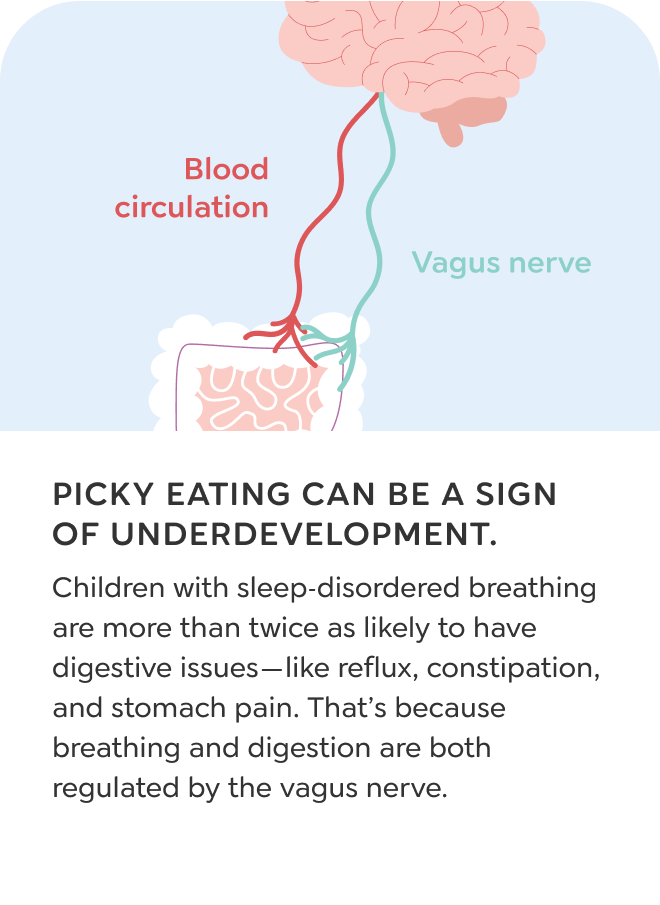
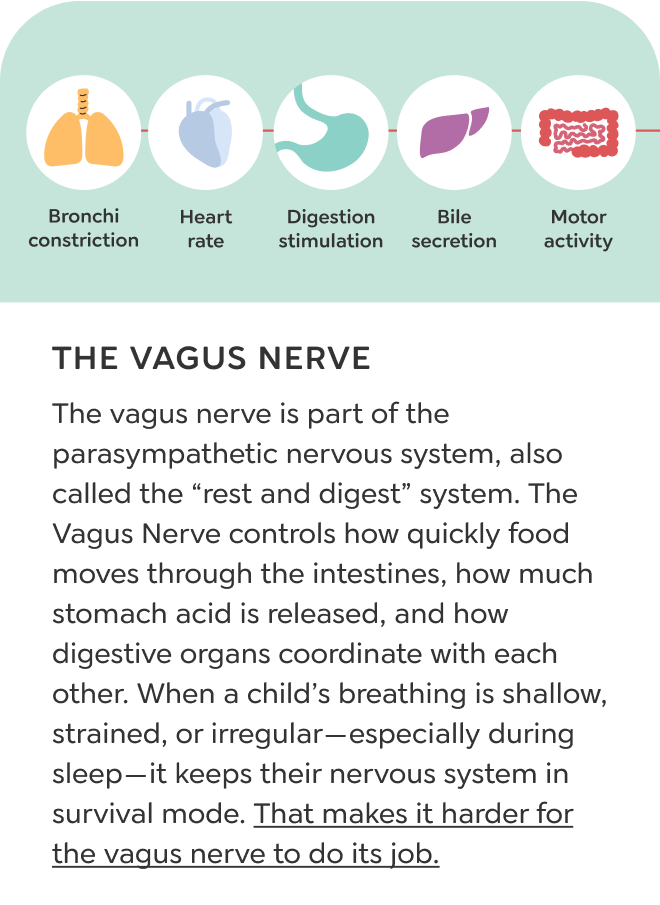
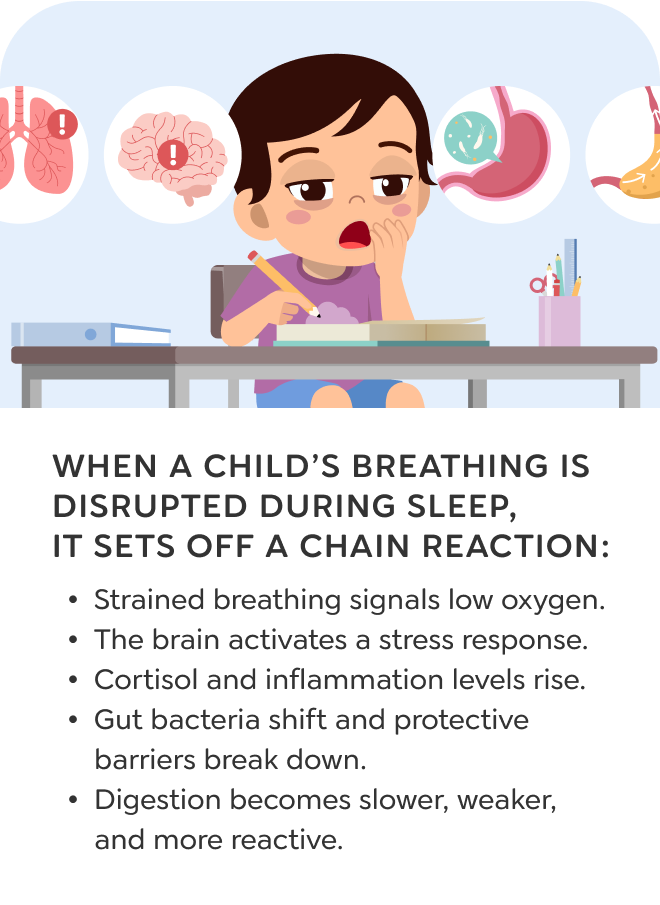
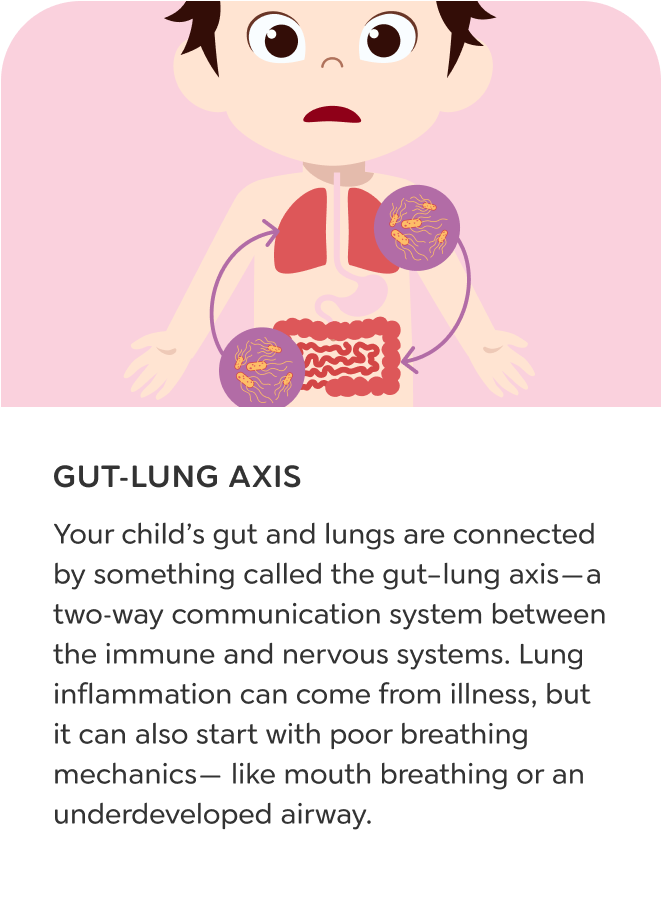
Reflux, constipation, bloating, and stomach pain are not always rooted in the gut. In children with disrupted breathing and poor jaw growth, these symptoms often begin higher up in the airway and nervous system.
Small jaws and low tongue posture can interfere with both breathing and swallowing. When the tongue cannot seal against the palate, children often swallow excess air throughout the day and night. This air fills the stomach and creates pressure throughout the digestive tract. At the same time, poor sleep and oxygen restriction disrupt the parasympathetic nervous system, which is responsible for regulating digestion during rest. The result is a system that cannot fully enter repair or processing mode.
The airway and gut work in constant communication. When breathing is shallow, strained, or mouth-based, digestion slows down. These children may experience frequent reflux, abnormal stool patterns, food sensitivities, or inflammation. Improving airway function can help restore balance to the digestive system.
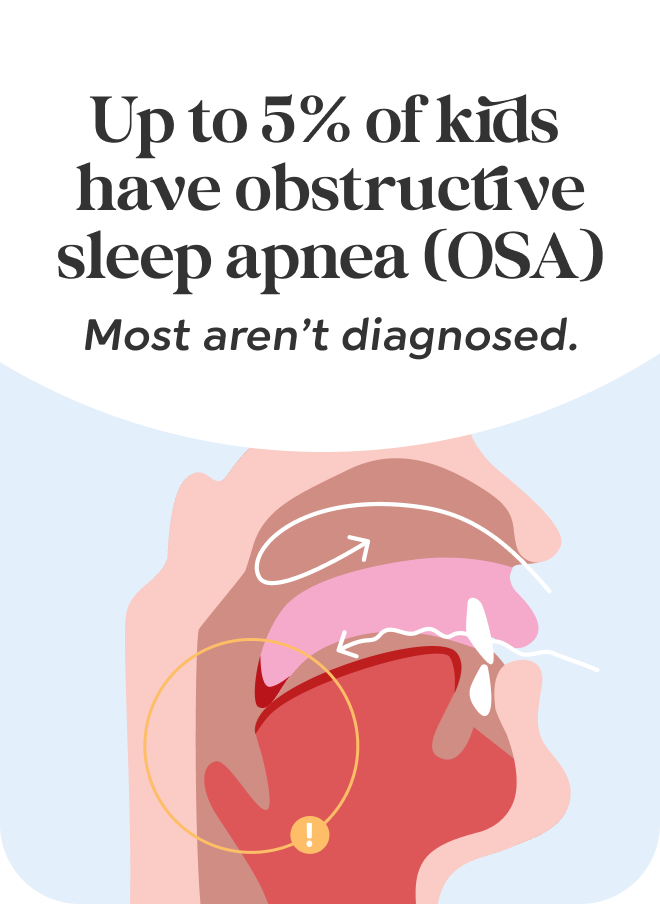
SLEEP APNEA
My child was diagnosed with sleep apnea!
Your child has been given a diagnosis, but the cause still feels unclear. Apnea doesn’t just appear. It’s usually tied to growth. Small jaws, poor tongue posture, or airway collapse can be part of the story.
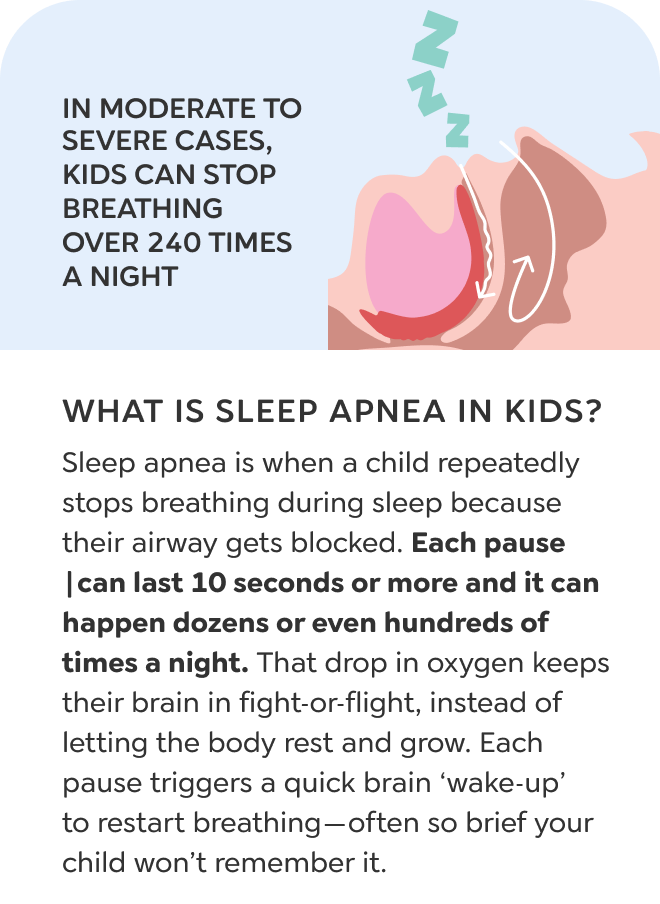
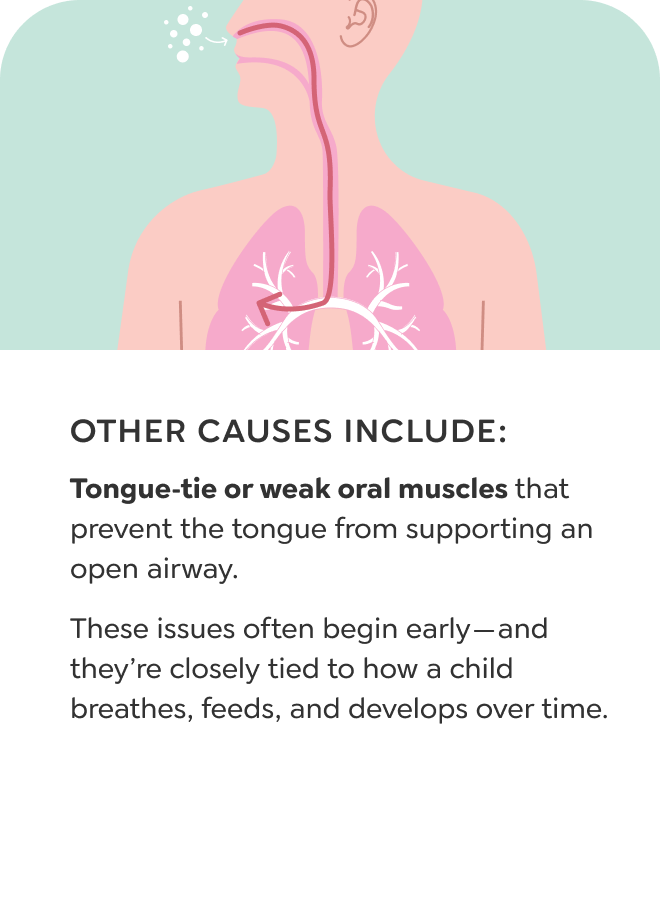
Sleep Apnea
Sleep apnea occurs when a child temporarily stops breathing during sleep. These pauses are often caused by airway collapse and can happen without gasping or choking. Instead, children may snore, sweat, grind their teeth, or move restlessly throughout the night. Each of these signs reflects a body that is struggling to maintain airflow while sleeping.
The most common reason for airway collapse is underdeveloped jaws. When the upper and lower jaws do not grow forward enough, the space behind the tongue stays narrow. During sleep, as the muscles relax, that space becomes even tighter. Airflow slows or stops, and the brain responds by interrupting sleep to protect breathing. These repeated arousals often go unnoticed but prevent deep, restorative rest.
While only a small percentage of children meet the criteria for a sleep apnea diagnosis, many more are on the same path. Mouth breathing, snoring, and disrupted sleep are early signs of an airway that is too small. Without proper growth, the risk of long-term sleep and breathing problems increases over time.
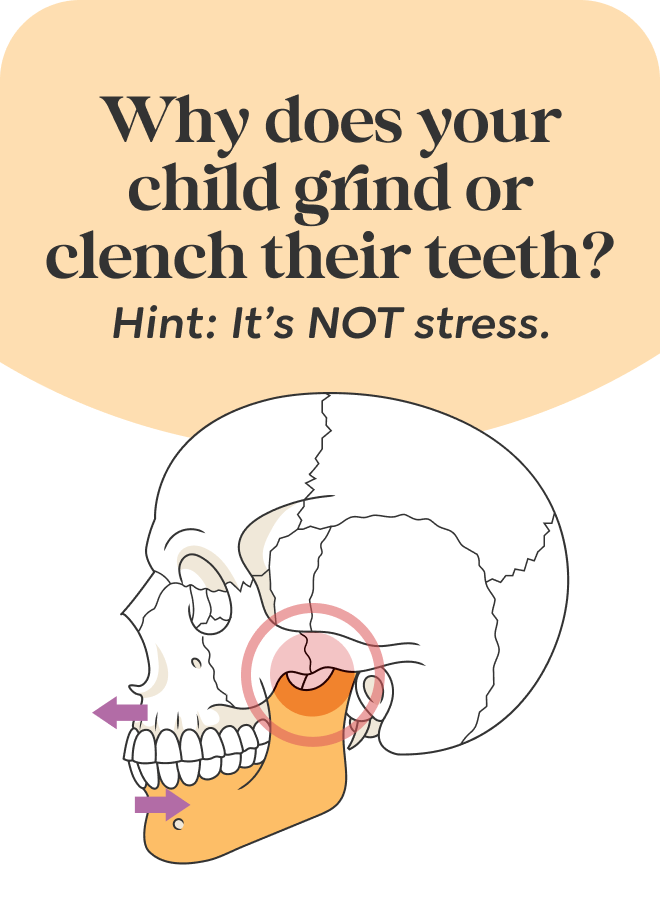
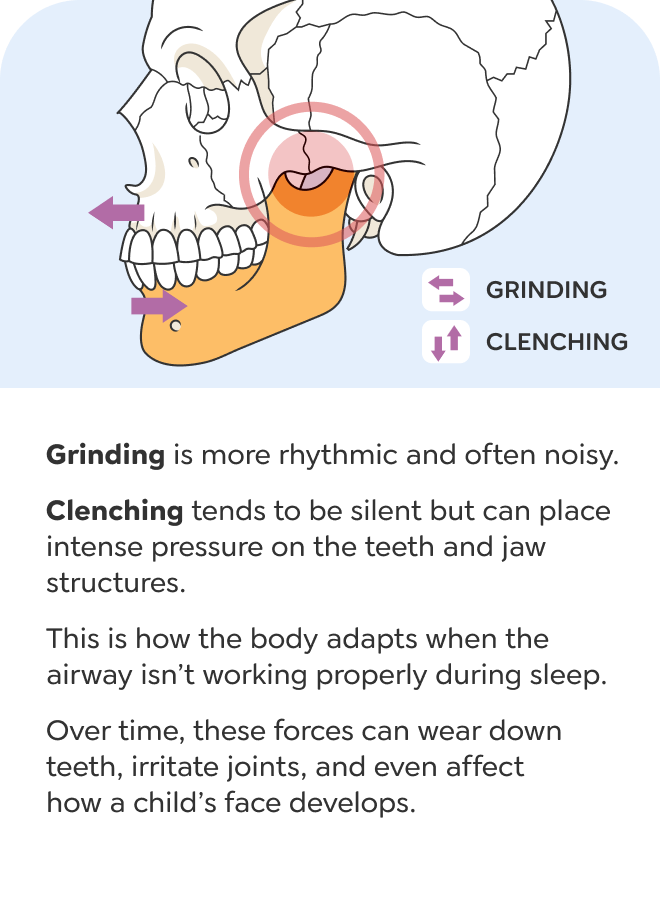
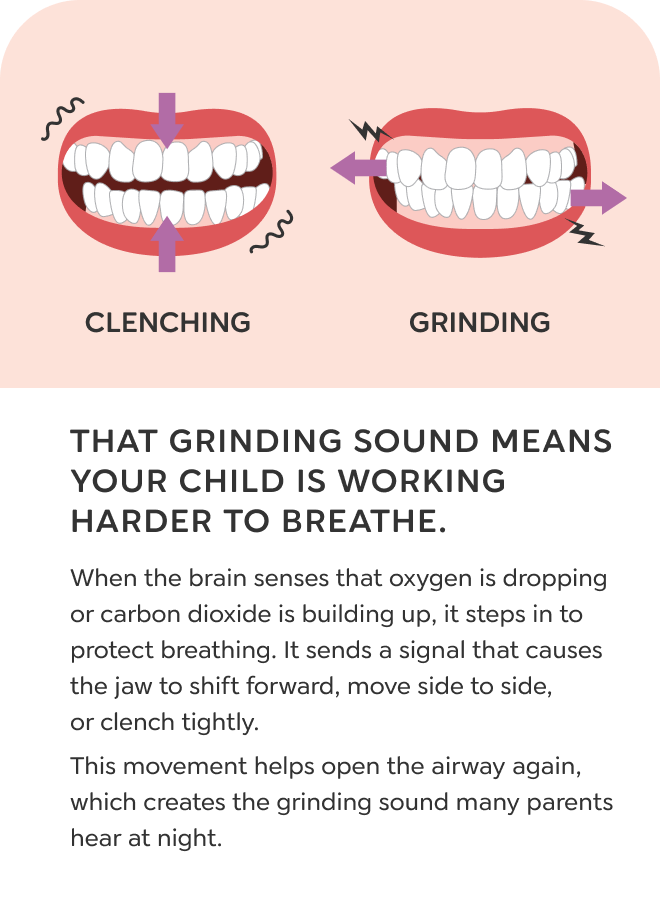
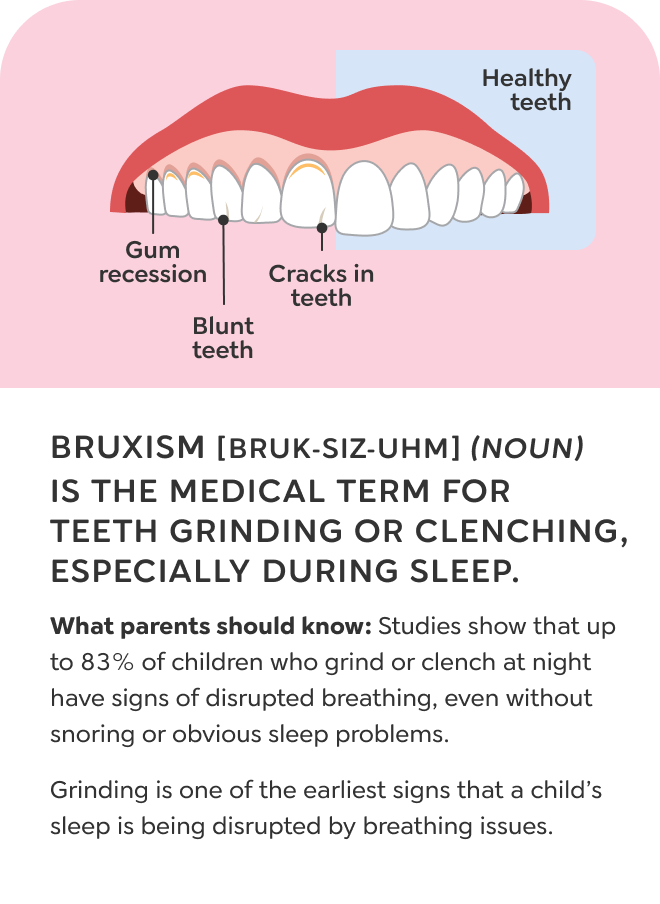
GRINDING / CLENCHING
My child grinds their teeth every night!
Your child clenches or grinds their teeth in their sleep, and it often sounds harsh or unsettling. This movement may be the brain's way of adjusting the jaw to open the airway and improve airflow during sleep.
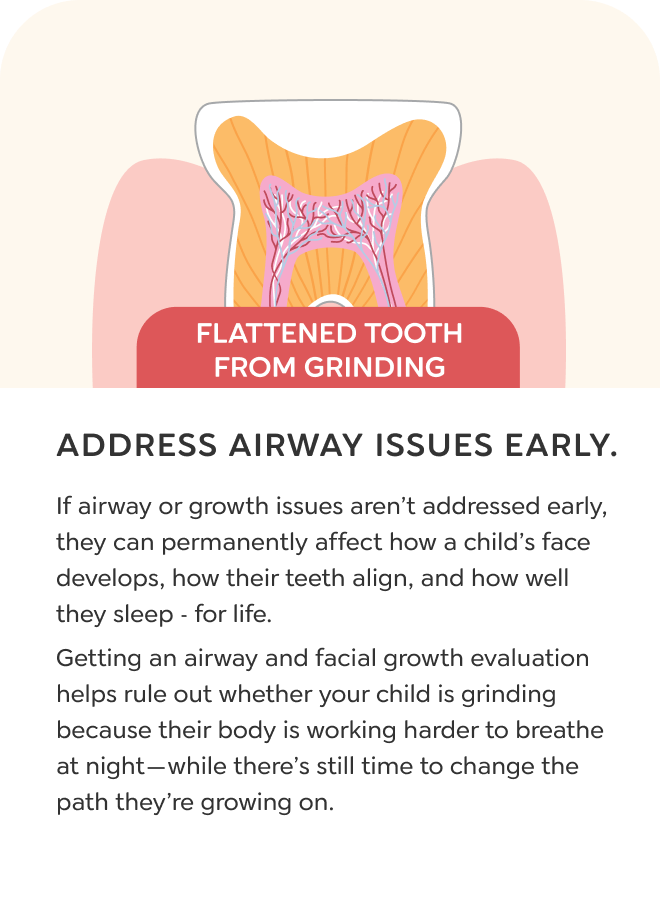
Grinding/Clenching
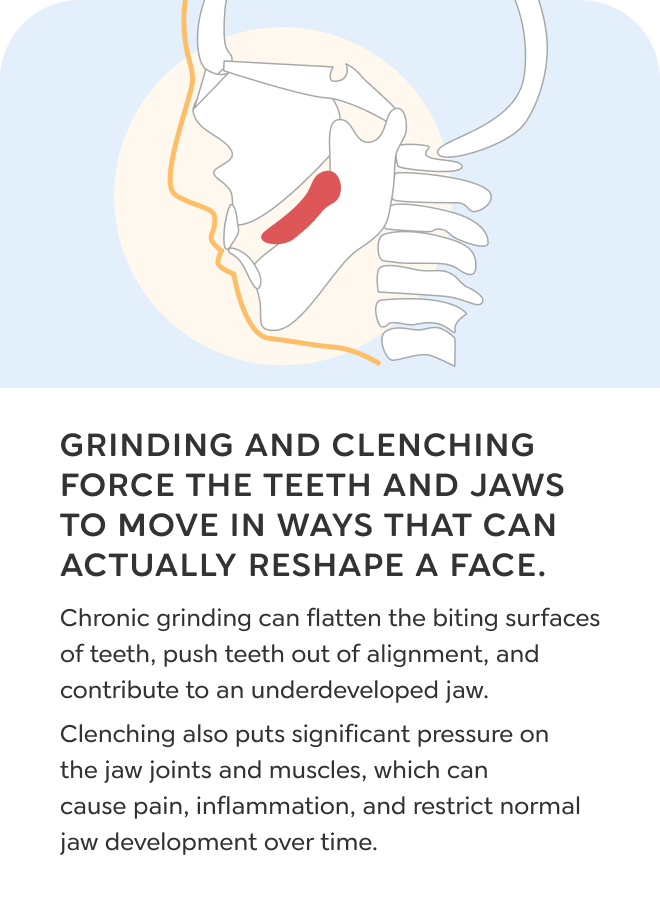
Grinding and clenching during sleep are often signs that a child is working hard to breathe. When the airway is narrow or unstable, the brain stays alert during sleep and activates the body to improve airflow. One of the ways it does this is by moving the lower jaw. That back-and-forth motion is what we recognize as teeth grinding.
The movement of the lower jaw also helps reposition the tongue. As the jaw shifts forward, the tongue moves with it, making it easier for air to pass behind it. Grinding is not a random habit or stress response. It is the brain’s attempt to maintain airflow when breathing is restricted.
Children who grind their teeth often have underdeveloped jaws, low tongue posture, or signs of mouth breathing. Each grinding episode reflects a disrupted airway during sleep. While it may help in the moment, ongoing grinding can lead to restless sleep, daytime fatigue, and long-term damage to the teeth or jaw joints.
MOUTH BREATHING
My child always breathes through their mouth!
Your child rarely keeps their lips closed, especially during sleep. Mouth breathing often happens when the nose is blocked or the jaws are too small. Over time, this can affect how the face and airway develop.
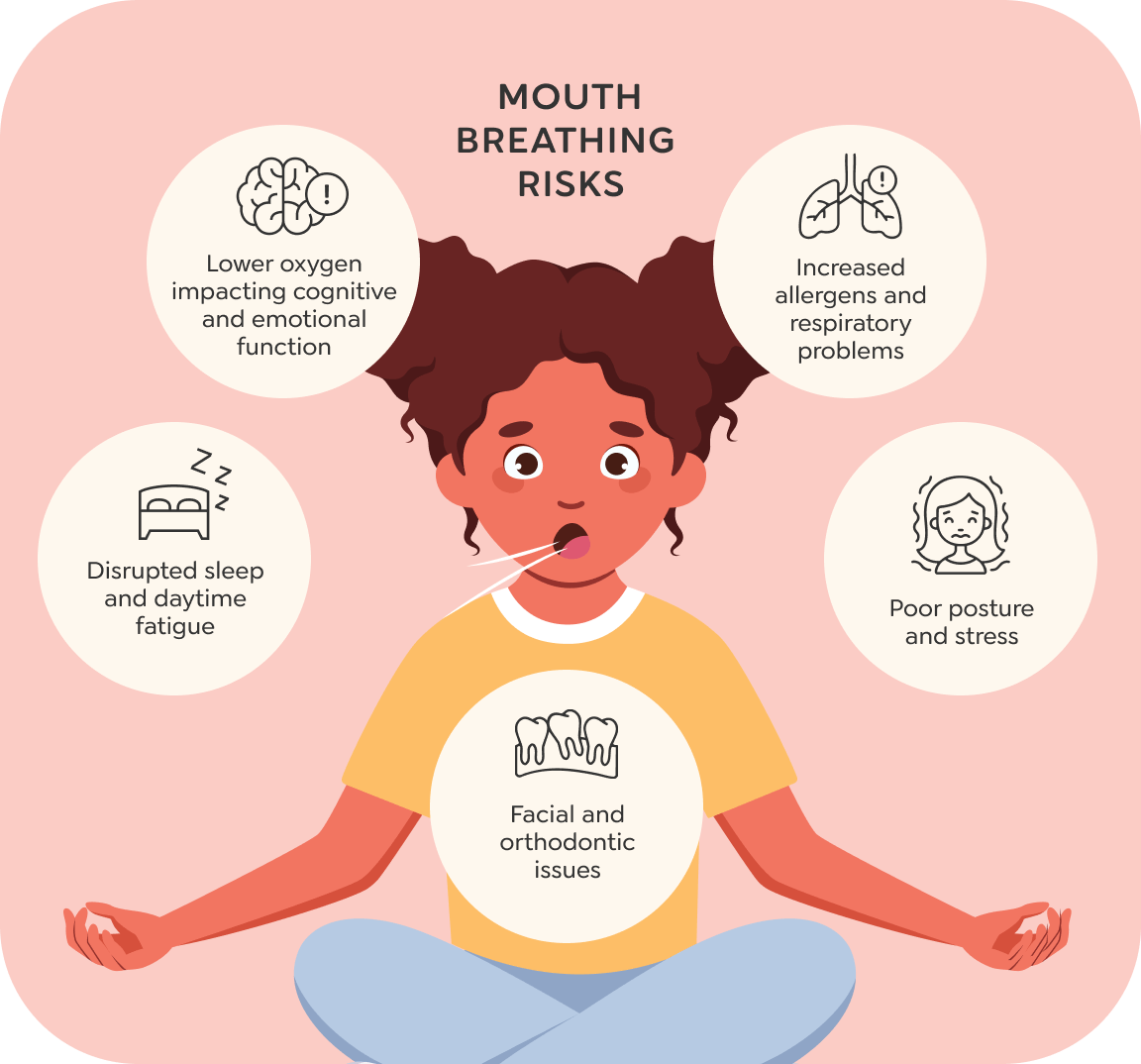
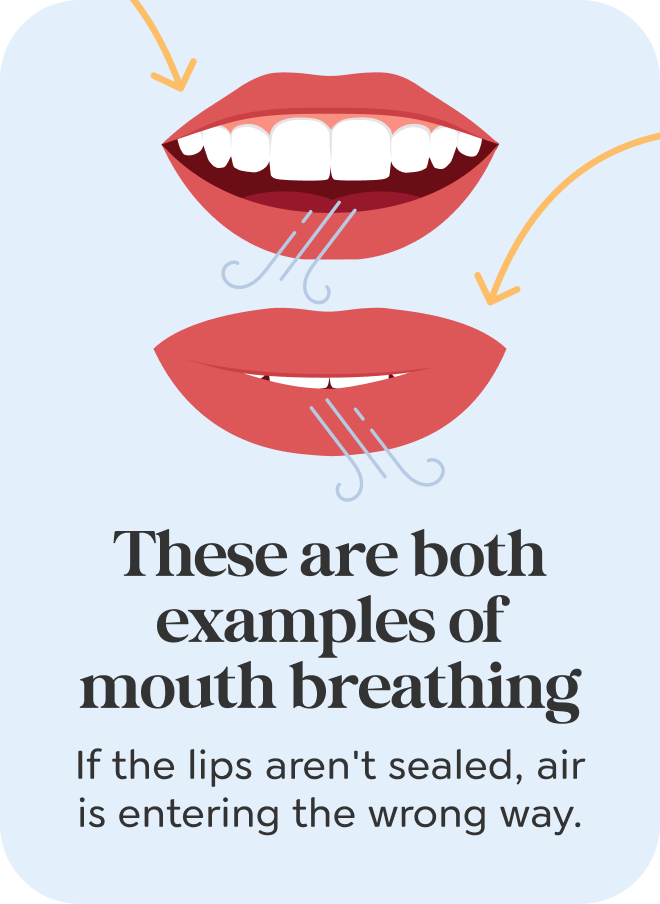
Mouth Breathing
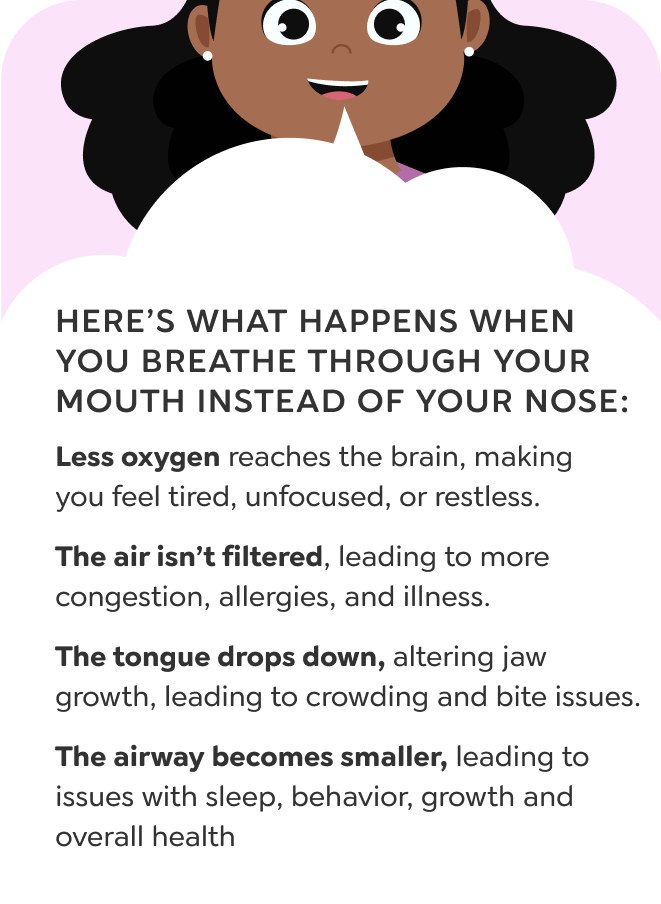
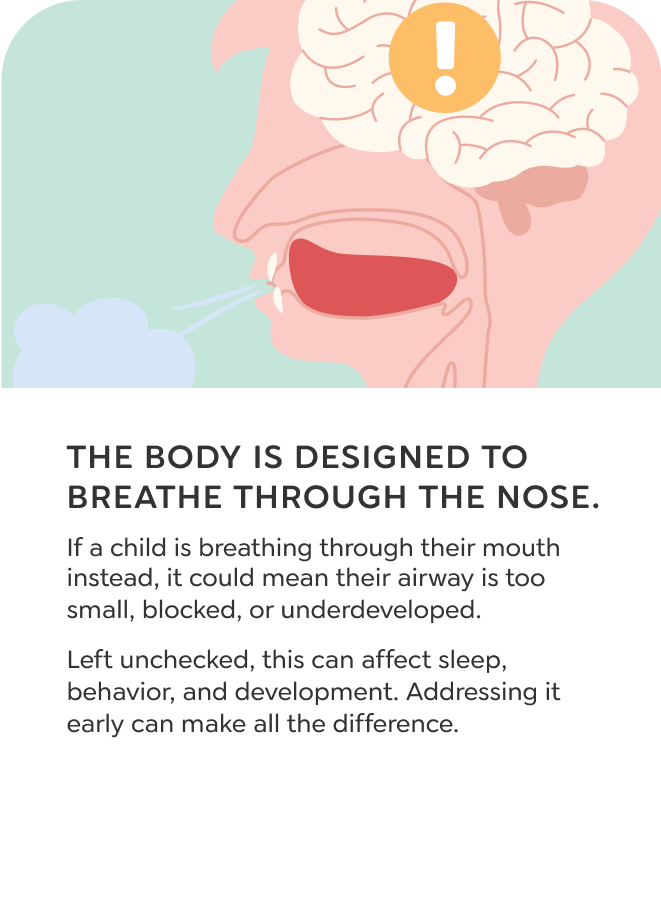
Mouth breathing happens when a child cannot get enough air through their nose. It is a physical compensation, usually caused by underdeveloped jaws, enlarged tissues, or chronic congestion that makes nasal breathing difficult. The lips separate, the tongue drops low, and air enters through the mouth instead of the nose.
Over time, this shift changes how the face grows. The tongue no longer supports the roof of the mouth, so the palate narrows, the upper jaw stays small, and the airway becomes more restricted. Children who breathe through the mouth are more likely to develop fatigue, poor focus, dry lips, bad breath, and symptoms that resemble ADHD or behavioral disorders.
The impact depends on how often it happens. A child who mouth breathes occasionally may show mild symptoms. A child who mouth breathes during both the day and night often experiences more serious effects on sleep, growth, and development. To correct it, the underlying reason for nasal obstruction needs to be identified and addressed.

An evaluation by an airway-focused dentist ensures accurate assessment and targeted support for your child's breathing and developmental needs.
If this is important, why hasn’t my doctor mentioned it?
Most medical and dental professionals have not received specialized training in airway airway or jaw development may need support.
This often leads to airway concerns being overlooked or misdiagnosed. Children experiencing airway-related symptoms are frequently advised to "wait and see," delaying proper intervention.
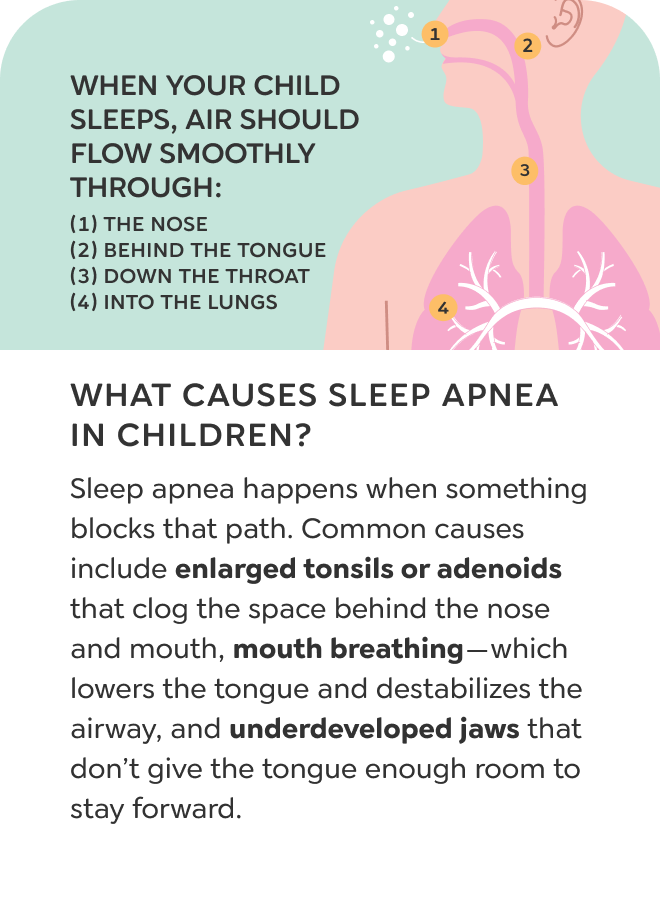
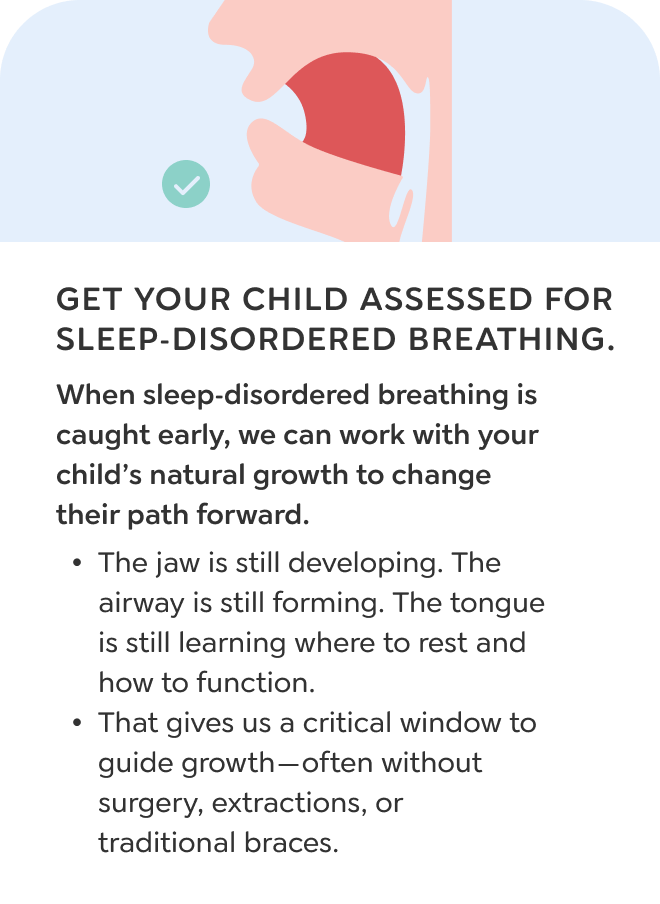
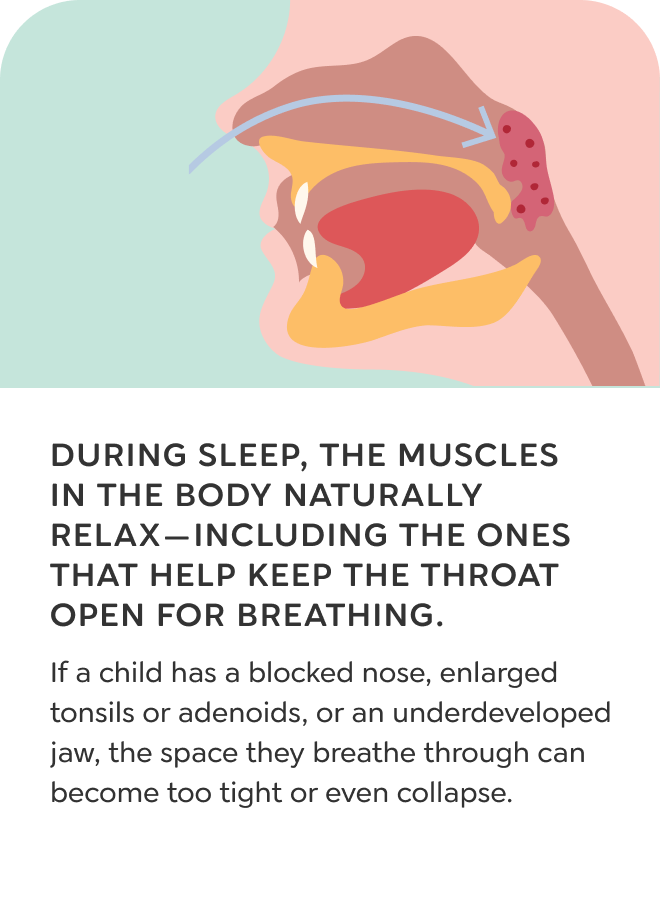
What happens during sleep?
During deep sleep, your child’s tongue should rest against the roof of the mouth, helping keep the airway open. But when the jaw is underdeveloped, the tongue falls backward, shrinking the airway and leading to disrupted breathing
The roof of your child’s mouth is also the floor of their nasal cavity.

Explore how early airway intervention reduces the need for future orthodontics.
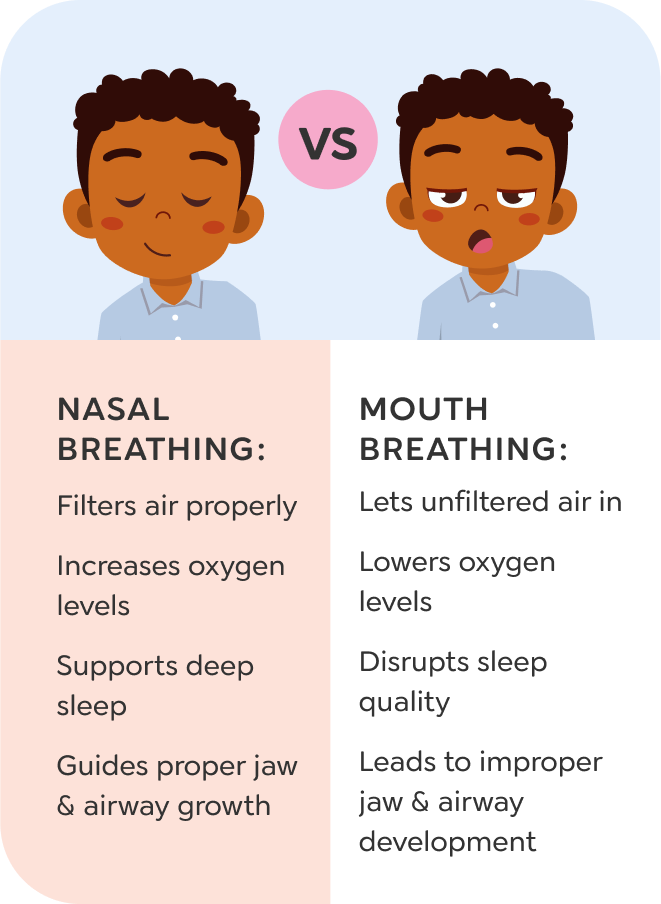
Help My Child Avoid BracesHow should a child breathe?
Children should breathe primarily through their noses. Nasal breathing filters air, optimizes oxygen absorption, and supports ideal facial growth.
Everyday struggles could be signs of an airway issue.
If your child shows even one of these signs, our free virtual assessment can help clarify what’s going on—and how to support their growth and breathing.
Start assessmentThe Toothpillow Program
Helping Kids Breathe, Sleep, and Grow the Way They Were Meant To.
Toothpillow is a dentist-guided airway program that helps your child grow in a way that supports better breathing, deeper sleep, and healthier development—without surgery or traditional braces. Proactive and family-friendly, it addresses root causes like jaw growth, tongue posture, and nasal breathing instead of just masking symptoms.
Learn more about the Toothpillow program
Free Virtual Assessment
Expert evaluation of airway and jaw health.

Customized Treatment Plan
Personalized structured plan.

At-home Guides and Therapy
Easy-to-follow exercises and tools.

Ongoing Expert Support
Continuous guidance and monitoring.

What you’ll learn from
the assessment:
Is your child’s jaw developing properly?
Could breathing be affecting their sleep or focus?
Are their symptoms related to airway restriction?
What next steps make sense for your child’s needs?

Take the first step:
You don’t have to guess anymore. Let an expert look deeper and help you understand what’s really going on.
It’s free. It’s easy. It’s virtual.
What happens when the right support finally shows up.
Sometimes the hardest part is not knowing where to turn. These parents had questions no one could answer—until they learned how breathing and jaw development were affecting their child’s sleep, behavior, and health.
Watch their stories and see what changed once they found the right kind of help.

If you’ve been looking for answers, this is where to start.
If your child’s symptoms haven’t made sense until now, this is your chance to understand what’s really going on. A free virtual assessment will help uncover what’s been missed—and what you can do about it.
Still have questions? We've got you.

FAQs
Know what to expect.
From timelines to treatment steps, get clear answers to the most common questions families ask before getting started.
Explore FAQs
Inside the program
Understand the full process.
Discover what makes this program different—and why families choose it to support their child’s development from home.
See how it works
Meet the doctors
Get to know the team.
Every family is paired with a licensed airway dentist who’s trained to spot what others often miss. Meet the experts guiding your child’s growth.
Meet the team

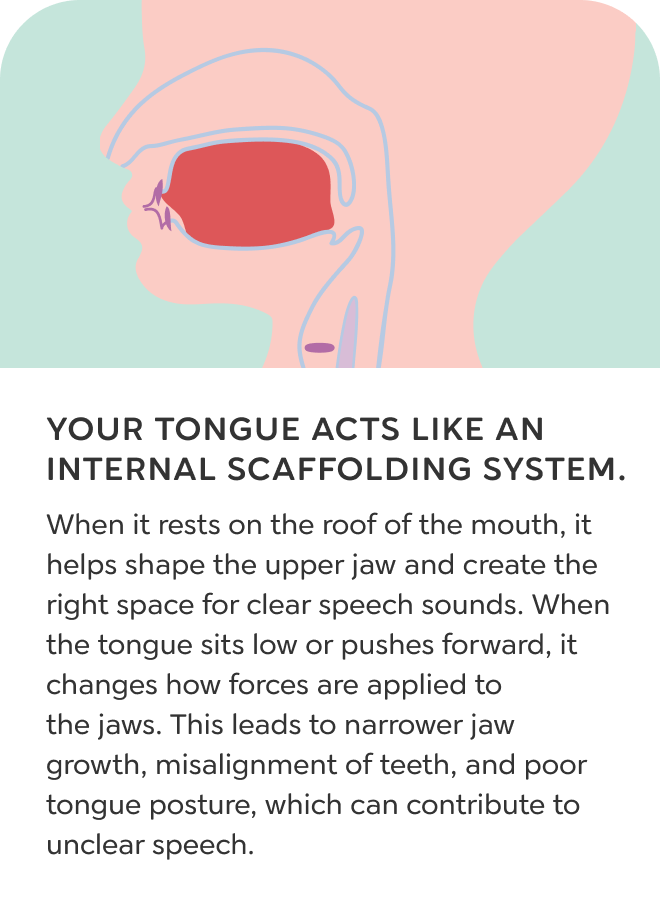




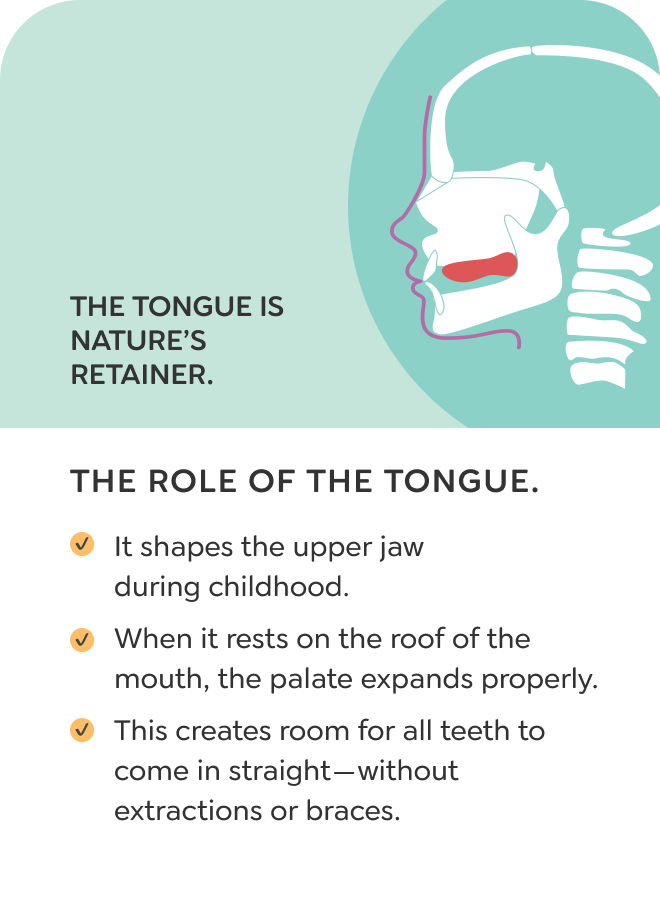










 Tongue rests on palate
Tongue rests on palate

 Tongue drops or falls back
Tongue drops or falls back

